|
 |
- Search
| J Acute Care Surg > Volume 9(2); 2019 > Article |
|
Abstract
A 19-year-old otherwise healthy male presented to the Emergency Department with left upper quadrant abdominal pain having felt a ŌĆ£popŌĆØ in his abdomen which was followed by nausea and lightheadedness. There was no evidence of trauma but 3 weeks earlier he began with symptoms of a sore throat and nasal congestion without cough. On subsequent investigation, given the patientŌĆÖs acute abdominal pain, abnormal vitals and a non-diagnostic computed tomography scan, an emergent exploratory laparotomy was performed. There was 600 mL of blood evacuated from the abdomen. A 643-gram inflamed and ruptured spleen was identified and removed, and follow-up lab work was positive for heterophile antibody. This report describes spontaneous splenic rupture caused by infectious mononucleosis and compares characteristics of traumatic versus non-traumatic cases.
Infectious mononucleosis is a common viral infection primarily caused by the Epstein-Barr virus (EBV). Symptoms typically begin from 4-6 weeks after EBV infection and include symptoms of a sore throat with swollen lymph nodes, extreme fatigue, fevers, head and body aches, hepatomegaly, splenomegaly and rash [1]. Infection occurs primarily through body fluids, sexual contact and fomites. In developing nations, > 90% of children have already been infected by EBV by 5-9 years of life, versus 50% of similar-aged children in developed nations [2]. In the United States, 82.9% of teens 18-19 years old tested seropositive for EBV [3], and only 25% of those infections develop into infectious mononucleosis [1]. Occurring in less than 0.5% of cases of infectious mononucleosis, splenic rupture is a rare complication [4]. The purpose of this study was to show that the course of a common illness can have important surgical consequences, and clinicians need to be alert to the presence of infectious mononucleosis, even in non-traumatic situations.
A 19-year-old otherwise healthy male presented to clinic with a 1-week history of a sore throat and nasal congestion without a cough. He was prescribed a course of Cefuroxime for acute rhinosinusitis but there was no improvement in his condition. Two weeks later, he was playing video games when he felt a mild ŌĆ£popŌĆØ in his abdomen followed by nausea and lightheadedness. He was evaluated in a local Emergency Department and sent home with amoxicillin after a positive rapid strep test. At home, his nausea and lightheadedness worsened and he developed left upper quadrant abdominal pain.
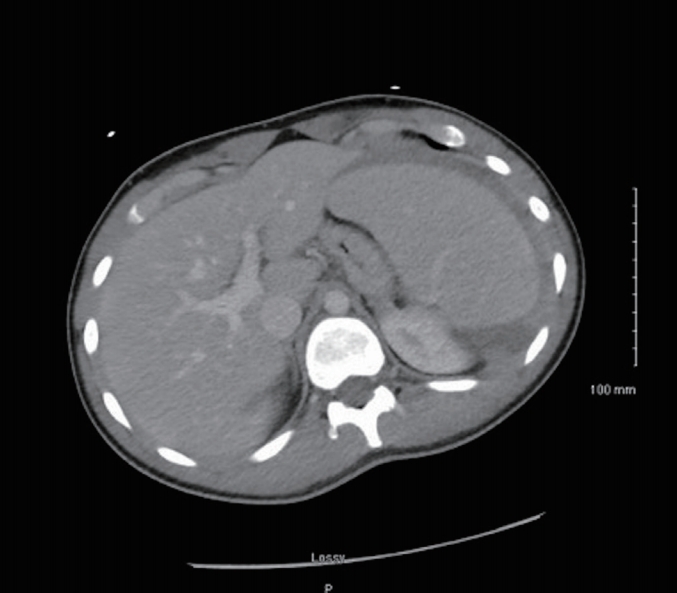
He presented at a second hospital, where his vital signs were measured. His pulse was 118 beats/min, respiration 21 breaths/min, blood pressure 107/64 mmHg, and his temperature was 36.6Ōäā. A physical examination showed a well-developed, pale and diaphoretic teenager in moderate distress, lying in a right lateral decubitus position. He was unable to lay in a supine position or change position. His abdomen was normal on inspection, with normal bowel sounds, and it was rigid with acute tenderness and guarding in all quadrants. There was no ecchymosis on his back. There was mild cervical lymphadenopathy and exudative tonsillar hypertrophy. Laboratory investigation revealed leukocytosis (8.7 109/L), normocytic anemia (hemoglobin 6.95 mMol/L) and mild hyperbilirubinemia (total bilirubin 41.04 ╬╝Mol/L) with normal transaminases. A computed tomography (CT) scan showed hepatosplenomegaly with a moderate amount of free fluid in the abdomen and pelvis, without the appendix being visualized (Figures 1 and 2).
Given the patientŌĆÖs acute abdomen, abnormal vitals, and non-diagnostic CT scan, an emergency exploratory laparotomy was performed. There was 600 mL of blood evacuated from his abdomen. An inflamed and ruptured spleen (643 g) was identified and removed (Figure 3), and follow-up lab work was positive for heterophile antibody. The post-operative recovery was unremarkable.
Unlike in traumatic splenic rupture, the mechanism of rupture in spontaneous cases is unknown. In a series of 613 patients, Aubrey-Bassler and Sowers reported that the most common categories in non-traumatic splenic rupture included infections (malaria, mononucleosis), followed by procedure-induced ruptures (colonoscopy), hematologic (lymphoma and leukemia) and cancers [5]. One study tested patients with confirmed mononucleosis and reported that they all had splenomegaly, suggesting this was a causal factor [6]. Histologically, splenomegaly is due to T and B cell infiltration and expansion of the red pulp of the spleen [7], which appears like a lymphoma. There are cases reported where vomiting, coughing, and even sneezing have been identified as triggers for the rupture of the spleen.
The use of a CT scan has allowed the emergence of non-operative management (waiting and angioembolization) of splenic injury in hemodynamically stable patients, when splenic pathology has been detected [8]. Using the American Association for the Surgery of Trauma (AAST) rating scale, grades of splenic injury correlate well with clinical outcome. Grade I is the least severe (a subcapsular hematoma occupying < 10% of surface area) and Grade V is the most severe (a shattered and/or devascularized spleen). As grades increase, the success of non-operative management decreases. In 1 study, Grade III injured spleens were associated with 19.6% of nonoperative failure versus a 75% failure rate in Grade V injured spleens. A successful non-operative approach was also associated with higher blood pressure, higher hematocrit and a lower quantity of hemoperitoneum. In this current case study, there was significant diagnostic and radiographic uncertainty preventing the use of the AAST rating scale. While the AAST rating scale is not well defined in cases of spontaneous splenic rupture (SSR), data shows that contrast-enhanced ultrasound provides an equivalent grading scale regardless of cause [9]. This same study also reported that, compared with traumatic splenic rupture (TSR), those with SSR were on average 62 versus 44 years old, and had a 4-week mortality of 36% vs 0% [9].
For acute care surgeons, it is important to be aware of organ ruptures in non-traumatic settings. To that end, 1 case series reported 85 cases of mononucleosis requiring splenectomy from 1984 to 2014, where only 14% of patients had a prior history of trauma leading to splenic rupture [10]. They observed that 70% were male with an average age of 22. Abdominal pain was the presenting complaint in 88% of cases and 67% required a splenectomy. The mortality rate was 9% for SSR [10]. In comparison, the mortality rate from TSR was reported retrospectively in 15,388 cases [11]. Patients with isolated splenic injury of AAST Categories I and II, III, IV, and V had 6.9%, 7.1%, 9.4%, and 22.7%, mortality rate, respectively, with an average of 8.3% across all groups [11]. The mortality risk of TSR appears similar to that of rupture due to mononucleosis, whereas mortality from other causes of SSR may be far greater [9].
Figure┬Ā1.
Transverse section of computed tomography with contrast showing hepatomegaly and splenomegaly with surrounding free fluid vs edema.
References
1. Epstein-barr | Mononucleosis | About Mono | CDC [Internet]. [cited 2017 Oct 20]. Available from: https://www.cdc.gov/epstein-barr/about-mono.html.
2. Takeuchi K, Tanaka-Taya K, Kazuyama Y, Ito YM, Hashimoto S, Fukayama M, et al. Prevalence of Epstein-Barr virus in Japan: Trends and future prediction. Pathol Int 2006;56(3):112ŌĆō6.


3. Dowd JB, Palermo T, Brite J, McDade TW, Aiello A. Seroprevalence of Epstein-Barr Virus Infection in U.S. Children Ages 6-19, 2003-2010. PLOS ONE 2013;8(5):e64921.



4. Jenson HB. Acute complications of Epstein-Barr virus infectious mononucleosis. Curr Opin Pediatr 2000;Jun;12(3):263ŌĆō268.


5. Aubrey-Bassler FK, Sowers N. 613 cases of splenic rupture without risk factors or previously diagnosed disease: a systematic review. BMC Emerg Med 2012;12:11.




6. Dommerby H, Stangerup SE, Stangerup M, Hancke S. Hepatosplenomegaly in infectious mononucleosis, assessed by ultrasonic scanning. J Laryngol Otol 1986;100(5):573ŌĆō9.


7. Sili├®zar MM, Mu├▒oz CC, Solano-Iturri JD, Ortega-Comunian L, Mollejo M, Montes-Moreno S, et al. Spontaneously Ruptured Spleen Samples in Patients with Infectious Mononucleosis Analysis of Histology and Lymphoid Subpopulations. Am J Clin Pathol 2018;150(4):310ŌĆō7.



8. El-Matbouly M, Jabbour G, El-Menyar A, Peralta R, Abdelrahman H, Zarour A, et al. Blunt splenic trauma: Assessment, management and outcomes. Surgeon 2016;14(1):52ŌĆō8.


9. Rosling M, Trenker C, Neesse A, G├Črg C. Spontaneous and Traumatic Splenic Rupture: Retrospective Clinical, B-Mode and CEUS Analysis in 62 Patients. Ultrasound Int Open 2018;4(1):E30ŌĆō4.


-
METRICS

-
- 2 Crossref
- 8,872 View
- 57 Download
-
Related articles in
J Acute Care Surg