Relevant Clinical Findings of Patients with Extraperitoneal Bladder Injury Associated with Pelvic Fracture Who Underwent Operative Management: A 6-Year Retrospective Study
Article information
Abstract
Purpose
Management options for extraperitoneal bladder injury (EBI) associated with pelvic fracture are variable. Predictive factors of operative management (OM) in patients with EBI associated pelvic fracture have not been previously addressed. This study assessed the current epidemiology of blunt traumatic urinary bladder injury and evaluated relevant clinical findings of patients with EBI associated with pelvic fracture who received OM.
Methods
Patients with urinary bladder injury with or without pelvic fracture from blunt trauma from January 1, 2014 to December 31, 2019 were identified from the institute trauma registry (n = 12,891). Demographics, mechanism of injury, type of urinary bladder injury, pelvic fracture configuration, and management options were analysed in the study population (n = 9,894).
Results
Of the 1,400 patients who had pelvic and/or acetabular fracture, 32 (2.3%) had urinary bladder injury. Of the 8,494 patients without pelvic and/or acetabular fracture, 12 (0.1%) had non-pelvic fracture urinary bladder injury. The total incidence of urinary bladder injuries in the study population was 0.4% (44/9,894). Patients with EBI associated with pelvic fracture who underwent OM, had a higher frequency of high-grade pelvic injury (100% vs 0%, p = 0.015), concomitant pelvic surgery (75.0% vs 0%, p = 0.001), and non-lateral compression type pelvic fracture (62.5% vs 10.0%, p = 0.043) compared with patients who underwent non-operative management of EBI.
Conclusions
These data suggest that OM may be considered especially in patients with EBI associated with pelvic fracture with high grade pelvic injury, concomitant pelvic surgery, and non-lateral compression type pelvic fracture.
Introduction
Pelvic fractures are often caused by high-energy events. The most common causes of pelvic fractures include motor vehicle collisions, motorcycle collisions, auto-pedestrian collisions, and falls from heights [1–3]. Urinary bladder injury is associated with pelvic fracture, thus mortality rates associated with bladder injuries are high (22%). Overall, approximately 60% of bladder injuries are extraperitoneal, 30% intraperitoneal, and 10% occur concomitantly [4–6].
Extraperitoneal injury is usually associated with the posterior bladder wall and fibrous attachments including the pubovesical ligament, puboprostatic fascia in men, superior fascia, and inferior fascia [7]. Although previous data has suggested that conservative care with catheter drainage and follow-up imaging is the treatment of choice, for most injuries for patients with an uncomplicated extraperitoneal injury, the current predictive factors and indication of operative management (OM) of extraperitoneal bladder injury (EBI) have not been fully evaluated [7,8]. The evaluation and clinical management of EBI with pelvic fractures are variable [9–11].
In this study urinary bladder injury in a single-institution, over 6 years was reviewed. The aim of this study was to determine the current epidemiology of bladder injury management, and to assess relevant clinical findings of patients with EBI associated with pelvic fracture who underwent OM.
Materials and Methods
1. Study setting
A retrospective study was performed using medical data from a regional trauma center between January 1, 2014 and December 31, 2019. Patients were identified using the hospital inpatient enquiry system. Data was retrospectively reviewed from the medical records and included a total of 12,891 patients with traumatic injuries admitted to the trauma centre. This project was exempt from the Institutional Review Board review of Pusan National University Hospital. Signed informed consent from the patients was not required.
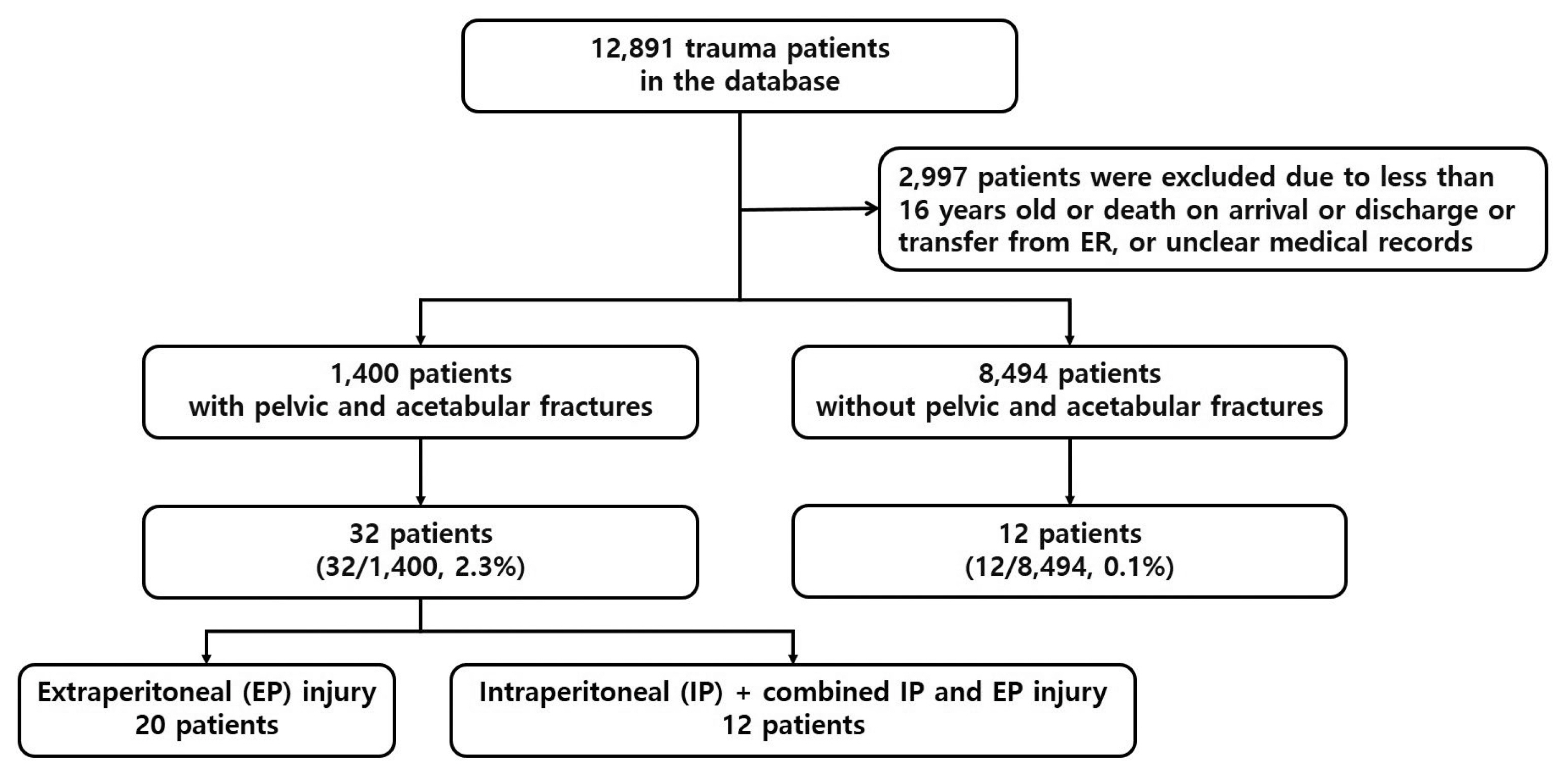
All patients with urinary bladder injury were included. The exclusion criteria were < 16 years old, declared dead on arrival, discharged/transferred from the emergency room, or unclear medical records. The final study population included 44 patients with urinary bladder injuries (Figure 1). Patient demographics, mechanism of injury, and details of injuries were included in this study (age, sex, mechanism of injury, vital signs on arrival, Abbreviated Injury Scale score, Injury Severity Score, shock index, length of hospital stay, intensive care unit (ICU) length of stay (LOS), and survival status).
2. Injuries recorded
2.1. Urinary bladder injury
The demographics of patients with urinary bladder injury, with and without pelvic fractures were included. The association between urinary bladder injuries and the type of pelvic fracture was also investigated. Bladder injuries were graded according to the American Association for the Surgery of Trauma Organ Injury Scale classification system [12].
2.2. Orthopaedic injuries
Pelvic fracture (a pelvic ring fracture and/or acetabular fracture) details, including the fracture type according to the Young and Burgess [13,14] and Tile [15] classifications for pelvic fractures were included. The Young and Burgess system classifies pelvic fractures into lateral compression (LC) Types 1–3, anterior-posterior compression (APC) Types 1–3, vertical shear (VS), and combined mechanism (CM). The Tile system classifies fractures into Types A, B, and C. Pelvic fractures were subdivided into 3 broad categories: high-energy pelvic fractures, low-energy pelvic fractures, and isolated acetabular fractures. High-energy pelvic fractures were defined as LC3, APC3, VS, and CM types. Low-energy pelvic fractures were defined as LC1, LC2, APC1, and APC2. High-grade pelvic injury was defined as patients who had an Abbreviated Injury Scale ≥ 4 or a Tile system classification Type C in the pelvis.
3. Outcome measures
The primary objective was to assess relevant clinical findings of patients with EBI associated with pelvic fracture who underwent OM. The secondary objective was to report the mechanism, incidence, and extent of urinary bladder injuries with and without pelvic fracture.
4. Statistical analyses
Summary statistics are reported as the median and interquartile range (IQR) where appropriate. Categorical variables are expressed as number and percentage. The Mann-Whitney U test was used for comparisons of the median values of continuous variables and for ordinal data, respectively, whereas the chi-square test and Fisher’s exact test were used to compare frequencies of categorical variables between groups. A p < 0.05 was considered statistically significant. Stata Version 14.2 (Stata Corp., College Station, TX, USA) were used to analyse the data.
Results
1. Patient characteristics and clinical features of patients with urinary bladder injury
In total, 12,891 trauma patients were admitted to hospital during the 6-year study period. Of these, 2,997 patients met the exclusion criteria and 9,894 patients formed the final study population. Of the 1,400 patients with pelvic fractures, 32 had urinary bladder injuries (32/1,400; 2.3%). Of the 8,494 patients without pelvic fractures, 12 had urinary bladder injuries (12/8,494; 0.1%). The total incidence of urinary bladder injuries was 0.4% (44/9,894; Figure 1).
The median age of the patients with bladder injury was 55 years (IQR, 42–64) and the male to female ratio was 2.38:1. Pedestrian traffic accidents were the most common mechanism of injury, representing 34.1% of total cases. Combined bladder and urethral injuries occurred in 6 of 44 patients (13.6%). Of the 44 bladder injuries, 22 were classified as extraperitoneal bladder injuries (EBIs; 50.0%) and 19 as intraperitoneal injuries (43.2%). The remainder were classified as combined extraperitoneal and intraperitoneal injuries (n = 3, 6.8%). There were 3 Grade 4 bladder injuries, 33 Grade 3, and 8 Grade 2 injuries. Formal retrograde cystography was performed in 31.8% of bladder trauma cases during the initial hospitalization. Eight cases (18.1%) of bladder injury were diagnosed by intraoperative findings, with 27.2% consisting of EBIs (n = 6). The remainder were diagnosed by computed tomography (CT) findings (n = 22, 50.0%). All intraperitoneal ruptures and combined extraperitoneal and intraperitoneal injuries required emergency repair. Surgical repair of the urinary bladder consisted of a 2-layered closure technique, followed by an elective fluoroscopic cystogram after 14 days. In addition, 8 extraperitoneal ruptures required surgical repair; a bone fracture fragment penetrating the bladder (n = 3), planned orthopedic open fixation with permanent hardware to be exposed to the area of injury (n = 3), concomitant bladder neck or rectal injury (n = 1), and initial concern for intraperitoneal injury (n = 1). There were no complications in this cohort. The median length of hospital stay and ICU LOS were 28 days (IQR, 12–58) and 4 days (IQR, 1–14), respectively. Mortality during initial hospitalization occurred in 3 patients (6.8%). Detailed demographics of the patients with urinary bladder injury are summarized in Table 1.
2. Comparison of clinical features of patients with urinary bladder injury with and without pelvic fracture
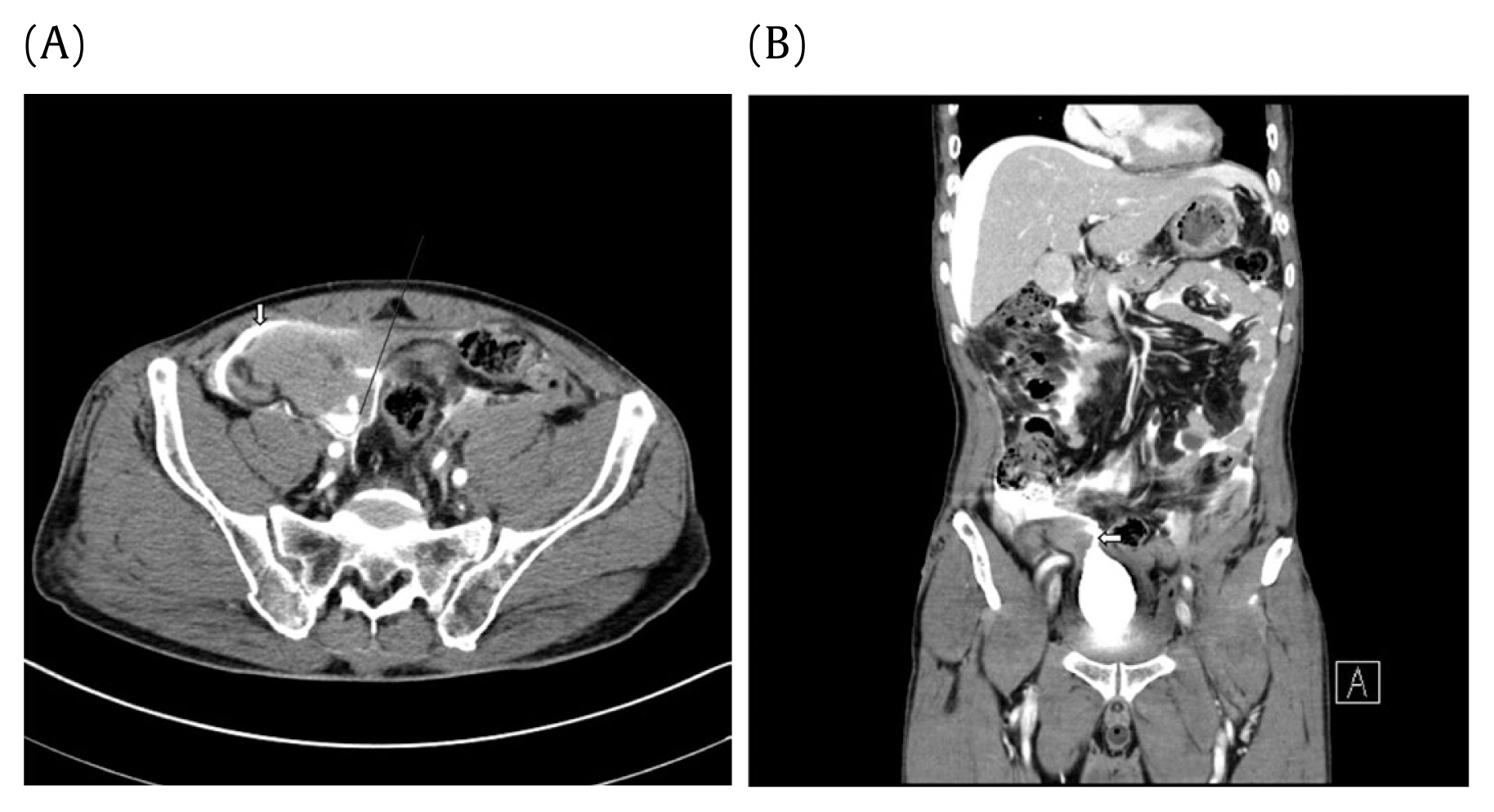
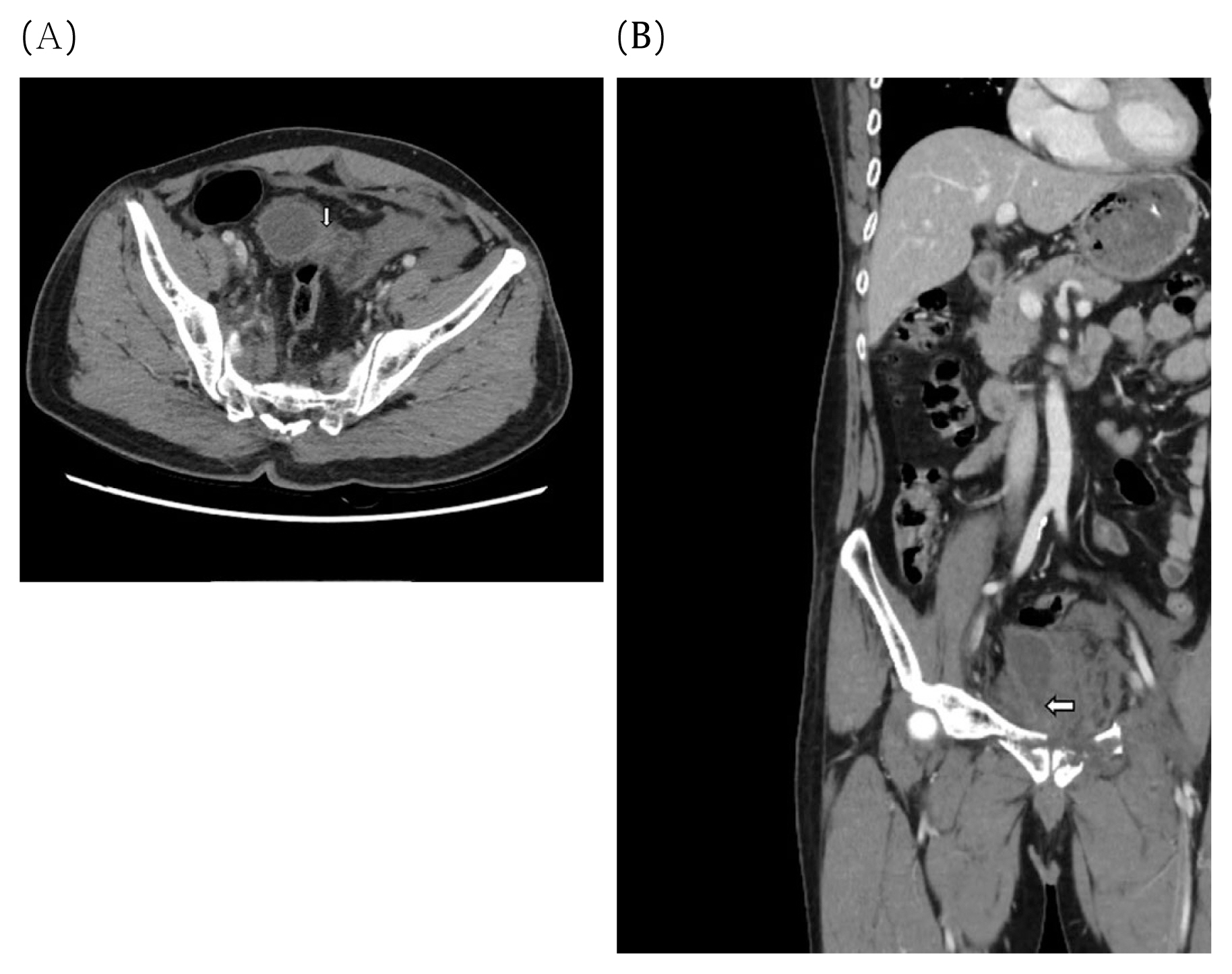
The clinical features of patients with urinary bladder injury with and without pelvic fracture are shown in Table 1. In patients with pelvic fractures, EBIs were the most common (62.5%; Figure 2), whereas intraperitoneal bladder injuries were the most common in patients without pelvic fractures (83.3%; p = 0.004; Figure 3). A comparison of the pelvic fracture and non-pelvic fracture groups revealed that patients with pelvic fractures had a lower systolic blood pressure upon arrival at hospital (p = 0.015), a higher Injury Severity Score (p < 0.001), longer length of hospital stay (p < 0.001), and longer ICU LOS (p = 0.003). However, age, sex, heart rate (upon arrival at hospital), shock index, Glasgow Coma Scale, and Revised Trauma Score were not significantly different when comparing with and without pelvic fracture groups. There was no difference in mortality between the 2 groups and the American Association for the Surgery of Trauma Organ Injury Scale used to grade bladder injury, was not associated with mortality.
Extraperitoneal bladder injury. (A) Axial CT imaging demonstrates extraperitoneal pelvic fluid collection. (B) Coronal CT imaging shows anteroinferior bladder injury.
CT = computed tomography.
3. Relevant clinical findings of patients with EBI associated with pelvic fracture who underwent OM ( = 20)
The relevant clinical findings of patients with EBI associated pelvic fracture who underwent OM are shown in Table 2. A comparison of the non-operative management (NOM) and OM groups revealed that patients who underwent OM had high-grade pelvic injury (p = 0.015), concomitant pelvic surgery (p = 0.001), and a higher frequency of non-LC type pelvic fracture (p = 0.043). However, there was no definitive association between a specific type of the Tile system classification (Type A, B, or C) and the type of fracture (high-energy pelvic fracture vs low-energy pelvic fracture).
4. Characteristics of patients underwent OM in patients with EBI associated with pelvic fracture ( = 8)
The characteristics of patients with EBI associated with pelvic fractures who received OM are shown in Table 3. Pedestrian traffic accidents and falls were the most common mechanism of injury, representing 75.0% of the total number of cases. There were 6 Grade 3 bladder injuries and 2 Grade 2 injuries. Concomitant urethral injuries occurred in 2 out of 8 patients (25.0%). Interestingly, all patients who underwent OM demonstrated gross hematuria and had a high-grade pelvic injury.
Discussion
This study is the first to evaluate the epidemiology of urinary bladder injuries in a large contemporary cohort of trauma patients in South Korea, and to examine the role that concomitant pelvic fracture has in influencing outcomes in management options. Although the bladder is relatively protected due to its anatomical location deep within the bony pelvis, injury may occur during severe pelvic trauma [16]. EBIs occur almost universally where there has been pelvic fracture [4,5]. However, intraperitoneal bladder injuries are most often due to blunt trauma to a distended bladder, resulting in elevated bladder pressure and perforation through the dome of the bladder [8]. The data in this current study support data that EBIs occur almost universally in the presence of pelvic fracture. In total, 62.5% of trauma patients with pelvic fractures had EBIs and 28.1% had intraperitoneal bladder injuries. On the other hand, the overall incidence of bladder injuries from blunt pelvic trauma was low (only 2.3% of all pelvic fractures), compared with previously reported data [4,16,17].
Intraperitoneal ruptures are almost universally treated operatively, whereas extraperitoneal ruptures are often managed nonoperatively. For patients with an uncomplicated extraperitoneal injury and pelvic fracture, a large bore (≥ 16 French scale) catheter used for 2–3 weeks without surgical intervention is the treatment of choice, as many of these injuries will heal without operative intervention [7,9–11]. Immediate surgical repair of an EBI is appropriate in the setting of intravesical bone spicules, rectal or vaginal laceration, and bladder neck injuries in order to minimize the risks of fistula formation, an abscess, urine leaks, and incontinence [9–11,18]. Immediate repair may also be considered for patients undergoing an exploratory laparotomy or an internal fixation of their pelvic fracture to minimize urine contamination of orthopedic hardware [8–11].
In contrast to previous studies, the study aimed to investigate relevant clinical findings of patients with EBI associated pelvic fracture who received OM. This retrospective study showed that high-grade pelvic injury, concomitant pelvic surgery, and non-LC type pelvic fracture are relevant factors for OM in the EBIs in the study patient population. It is not difficult to assume that a patient population with a more severe pelvic injury would have a greater likelihood of bladder involvement. However, in this current study population, interestingly high-grade pelvic injury resulted in OM in all patients with EBI associated with pelvic fractures who demonstrated gross hematuria
Using a mechanistic understanding of bladder injury, previous investigators have attempted to predict injuries based on particular fracture configurations [19–21]. Avey et al [21] showed in their cohort of 37 patients that symphysis pubis diastasis and obturator ring fractures with a displacement > 1 cm were independently associated with the risk of bladder injury. Bhatt et al [20] reported that bladder injuries occurred most frequently in high-energy pelvic fractures (LC3, APC3, and VS). However, these studies did not differentiate between intraperitoneal and EBI in terms of fracture patterns predicting injury [20,21]. The data in the current study shows LC and low-energy pelvic fracture were the most common fracture type (72.4% and 56.2%, respectively); however, there was no significant correlation between bladder injuries and a particular type of pelvic fracture. This is likely to be a result of the rarity of urinary bladder injury overall and lack of sufficient statistical power to detect a difference.
There are several limitations to this study. Firstly, the study was confined to patients who presented at a single regional trauma center so the study population may be regionally specific.. As such, the severity and frequency of injuries observed in this current study may differ significantly from those observed in a community emergency department. Secondly, as is true with most studies evaluating trauma, there was minimal follow-up data, which prevented assessment of long-term morbidity due to bladder injuries, and prevented the evaluation of differences in functional and patient-reported outcomes of OM and NOM groups. Lastly, because this was a retrospective analysis with a small sample size, the results observed in this study are not conclusive because they lack the sufficient statistical power to give meaningful results. Additional prospective studies with larger sample sizes are necessary to support the findings of this current study.
Conclusion
This study represents a single-institution cohort study collated for a 6-year period involving trauma patients with urinary bladder injuries. The results of this study suggests that OM should be considered for patients who present with EBI associated pelvic fracture, especially in those with high-grade pelvic injury, concomitant pelvic surgery, and non-LC type pelvic fracture, however, there are several limitations to the study. Further research involving a large-scale study is needed in order to clarify the relationship between management options and the EBI associated pelvic fracture.
Notes
Conflicts of Interest
No potential conflict of interest relevant to this article is reported.