Preventable Death Rate of Trauma Patients in a Non-Regional Trauma Center
Article information
Abstract
Purpose
A nationwide study (2012–2017) of preventable trauma death rates (PTDR) showed a 15.3% decrease after Regional Trauma centers were initiated. However, in non-trauma centers with an Emergency Department there is limited data of preventable mortality in trauma patients. Therefore, the purpose of this retrospective study was to investigate preventable mortality in trauma patients in a non-regional trauma center and determine the effect of initiating a Trauma Team.
Methods
There were 46 deaths of trauma patients recorded in the National Health Insurance service Ilsan Hospital (NHISIH) in South Korea from January 2019 to December 2021. These patients’ preventable deaths were analyzed by an expert panel review considering the implementation of the Trauma Team in April 2020.
Results
All deaths were attributable to blunt trauma with an average Injury Severity Score of 26.0 ± 19.2, Revised Trauma Score of 5.05 ± 3.20 and Trauma and Injury Score of 56.6 ± 41.3. The most frequent cause of death was traumatic brain injury followed by respiratory arrest. The most frequent error was delayed transfusion followed by delayed treatment of bleeding. Treatment errors occurred the most in the Emergency Room followed by the Intensive Care Unit. The PTDR of patients before the involvement of a Trauma Team (January 2019 to March 2020) and after the Trauma Team was initiated in April 2020 decreased from 27.27% to 4.27%, respectively (p = 0.021).
Conclusion
The introduction of a dedicated Trauma Team in a non-regional trauma center significantly reduced the overall PTDR in trauma patients.
Introduction
In 2012, the preventable trauma death rate (PTDR) in South Korea was 35.2% [1]. After the establishment of regional trauma centers, the PTDR in 2017 had reduced to 30.5%, and was further reduced to 19.9% by 2019 [2,3]. The PTDR can be used to evaluate the emergency medical system and to improve the quality of treatment for trauma patients. Preventable death in a trauma patient is defined as death that could be prevented if the patient had received the appropriate treatment and had arrived at a hospital within an appropriate time frame [4]. Regional trauma centers are hard to access in certain provinces because of distance or overcrowded with patients. [5]. In Korea, there are only advanced trauma life support (ATLS) Level I trauma centers, therefore, trauma patients might not be able to be sufficiently treated in non-regional trauma centers with Emergency Departments. A smaller Level II or III trauma center, or a Trauma Team in a regional emergency center, or a local emergency center, might help treat trauma patients not being able to be primarily treated at regional trauma center [2,6,7]. The National Health Insurance Service Ilsan hospital (NHISIH), a local emergency center without a Trauma Team formed a Trauma Team in 2020. Currently there are limited data of preventable deaths in trauma patients in local or regional emergency centers in South Korea. Therefore, the purpose of this study was to investigate preventable mortality in trauma patients in a non-trauma center, and the effect of introducing a Trauma Team.
Materials and Methods
1. Patient criteria
The individuals included in this study were trauma patients who died during treatment at the NHISIH between January 1st 2019 and December 31st 2021. The total number of trauma patients admitted during this period was 2,174 patients. Of those patients, 52 patients died. Through death panel review, 6 patients were excluded because they were non-trauma patients. There were 46 patients with trauma related deaths (Figure 1).
2. Preventable death panel review
Four general surgeons, who were members of the Trauma Team, were the expert panelists who reviewed the preventable deaths in trauma patients. The review criteria included time from injury to death, cause of death, quality and availability of information, severity of injury, quality of treatment, comorbidities, and other considerable factors (such as refusal of treatment by patient or patient’s family). The review by each expert was performed over 4 sessions with an average of 14 patient reviews per session. Each panelist made their own decision regarding the death of a patient before the review meeting and classified each trauma patient death as preventable (P), possibly or potentially preventable, non-preventable, or non-preventable, but with care that could have been improved. On the review meeting day, after deliberate discussion, a final review of preventable deaths in trauma patients was made with 100% consensus between experts.
3. Definitions
3.1. Trauma
Trauma was defined as injury caused by traffic accident including car, bicycle, motorcycle, pedestrian fall or slip, and penetrating injury.
3.2. Injury severity score
Injury severity score (ISS) is an anatomical scoring system that provides an overall score for patients with multiple injuries. Each injury is assigned an abbreviated injury scale (AIS) score and is allocated to one of 6 body regions. The highest AIS score in each body region is used [8].
3.3. Revised trauma score
Revised trauma score (RTS) is a physiologic-based triage score with a higher RTS is associated with a better chance of survival [9].
3.4. Trauma and injury score
Trauma and injury score (TRISS) is a combination index based on the RTS, ISS and the patient’s age [10].
4. Statistics
Categorical variables were compared using the chi-square and Fisher’s exact tests. Continuous variables were compared using Student t test and Mann-Whitney U test. Statistical significance was set at p < 0.05. All statistical analyses were performed using the Statistical Package for the Social Sciences (SPSS Version 23, IBM, Armonk, NY, USA).
5. Ethics approval
Ethical approval was obtained from the Institutional Review Board of the NHISIH (IRB no.: 2022-3-022-001).
Results
1. Patients characteristics
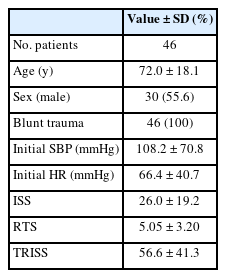
The average age of the trauma patients was 72.0 years-old and 55.6% were male. There was no penetrating trauma. The average initial systolic blood pressure and heart rate was 66.4 and 108.2 mmHg, respectively. The average trauma scores of ISS, RTS and TRISS were 26.0, 5.05, and 56.6, respectively (Table 1).
2. Time from injury to death
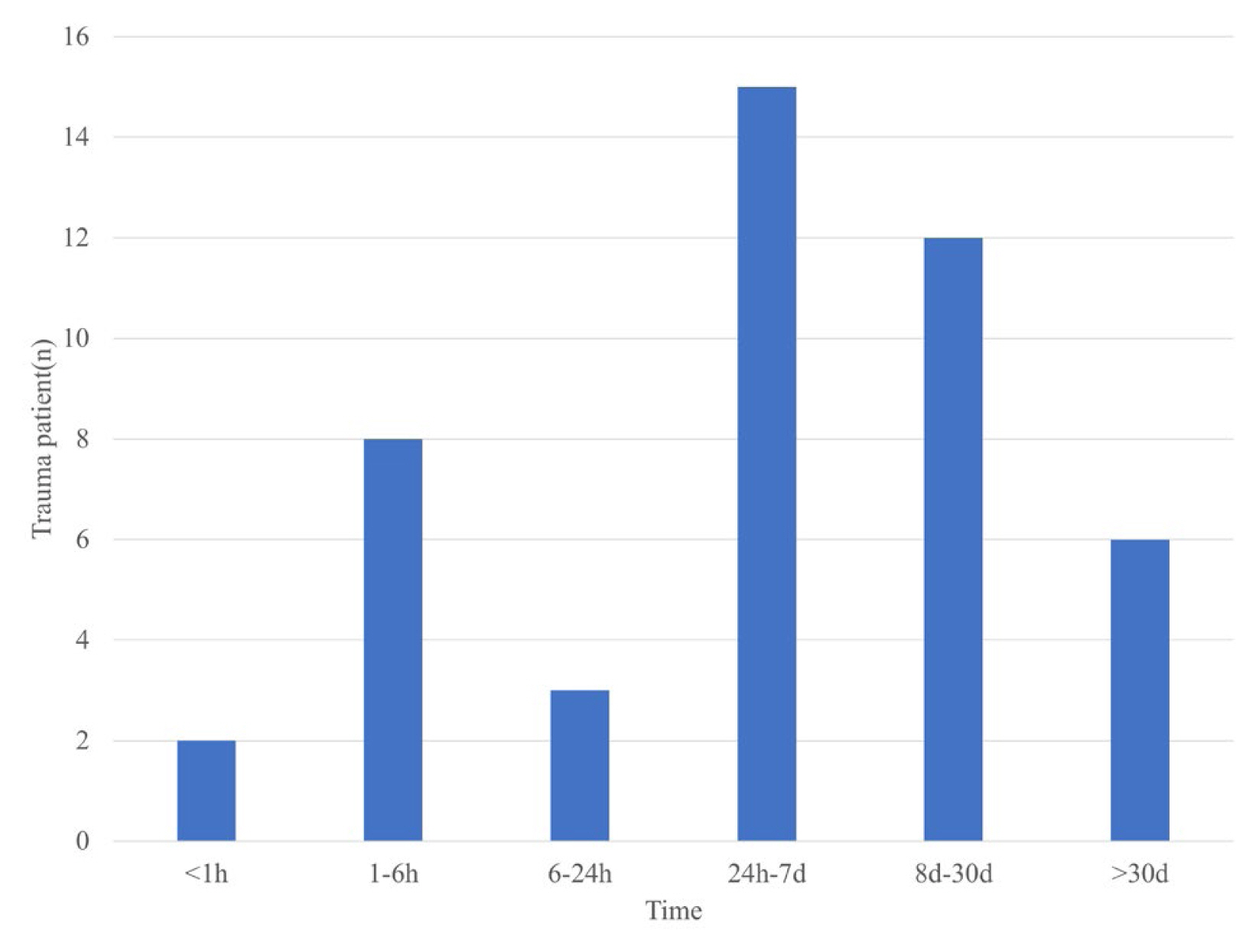
Most deaths occurred within 7 days (32.6%). The 2nd most frequent period of all deaths was 8–30 days (26.0%). Of note, 28.2% of patients died within 24 hours of trauma (Figure 2).
3. Cause of deaths
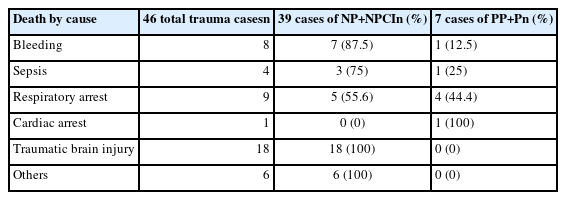
Of total trauma deaths, traumatic brain injury (TBI) related death was the most common cause of death (n = 18; 39.1%) followed by respiratory arrest (n = 9; 19.6%), and bleeding (n = 8; 17.4%). According to these 3 causes of death, preventable or possibly preventable death rates showed TBI had no cases affected (0%), respiratory arrest had 4 cases affected (44.4%), and bleeding had 1 case affected (12.5%; Table 2).
4. Shortcomings of treatment
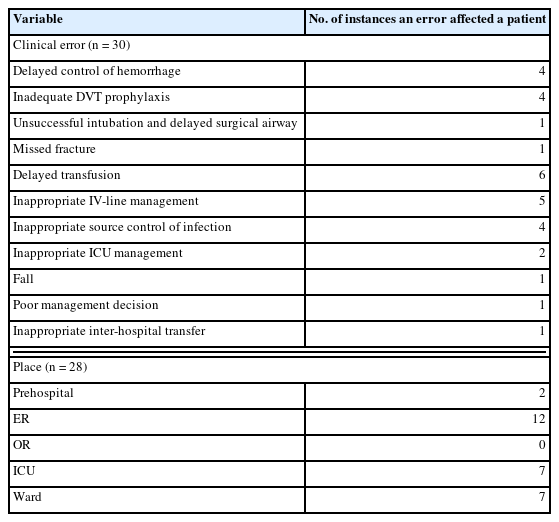
A total of 30 instances of an error were identified in 28 cases. The most common error was delayed transfusion in the Emergency Room (ER) where 6 (20%) cases were identified. The 2nd most frequent error was inappropriate intravenous (IV)-line management (16.7%). Referring to ATLS guidelines, this error included IV-line placement in lower extremities in unstable pelvic fracture patients rather than in the antecubital fossa of the arm, and not excluding central line catheters when line infections were suspected. Further frequent errors were delayed damage control of bleeding, inadequate prophylaxis of deep vein thrombosis (DVT), and inappropriate source control of infection excluding line infection (13.3%). According to location, there were 28 instances of an error occurring and the ER was where the most errors occurred (12 cases; Table 3).
5. Comparing preventable death rates before and after the implementation of the Trauma Team
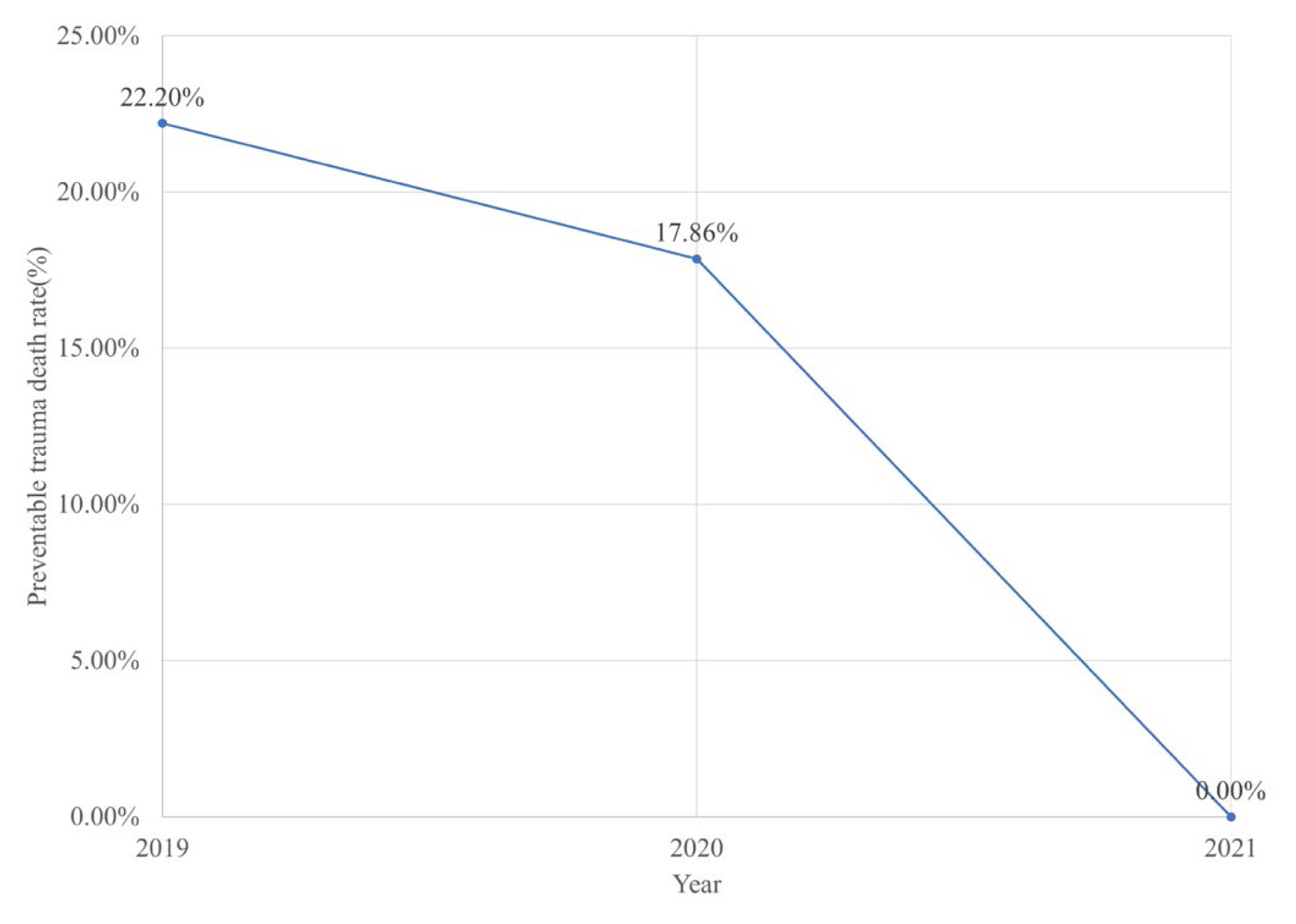
There were 46 trauma patients included in this study who died during treatment at the NHISIH between January 1st 2019 and December 31st 2021. The Trauma Team was initiated in May 2020. During the 14-month period without a Trauma Team (January 2019 to March 2020) 22 trauma patients died compared with 24 patients who died over the 18-month period (May 2020 to December 2021) after the Trauma Team was initiated. The preventable death rate decreased yearly from 2019 to 2021 (Figure 3) but without statistical significance (p = 0.35).
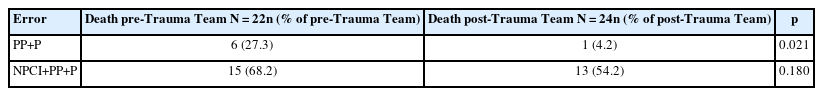
The PTDR before and after the implementation of a Trauma Team was compared. The PTDR due to preventable and possibly preventable error pre-Trauma Team was 27.27%, and the PTDR after the Trauma Team was initiated was 4.17%. The difference in PTDR between pre- and post-Trauma Team was statistically significant (p = 0.021; Figure 4). There was no statistical difference when comparing the total types of errors leading to death in trauma patients before and after the initiation of a Trauma Team, 68.2% and 54.2%, respectively (p = 0.15; Table 4).
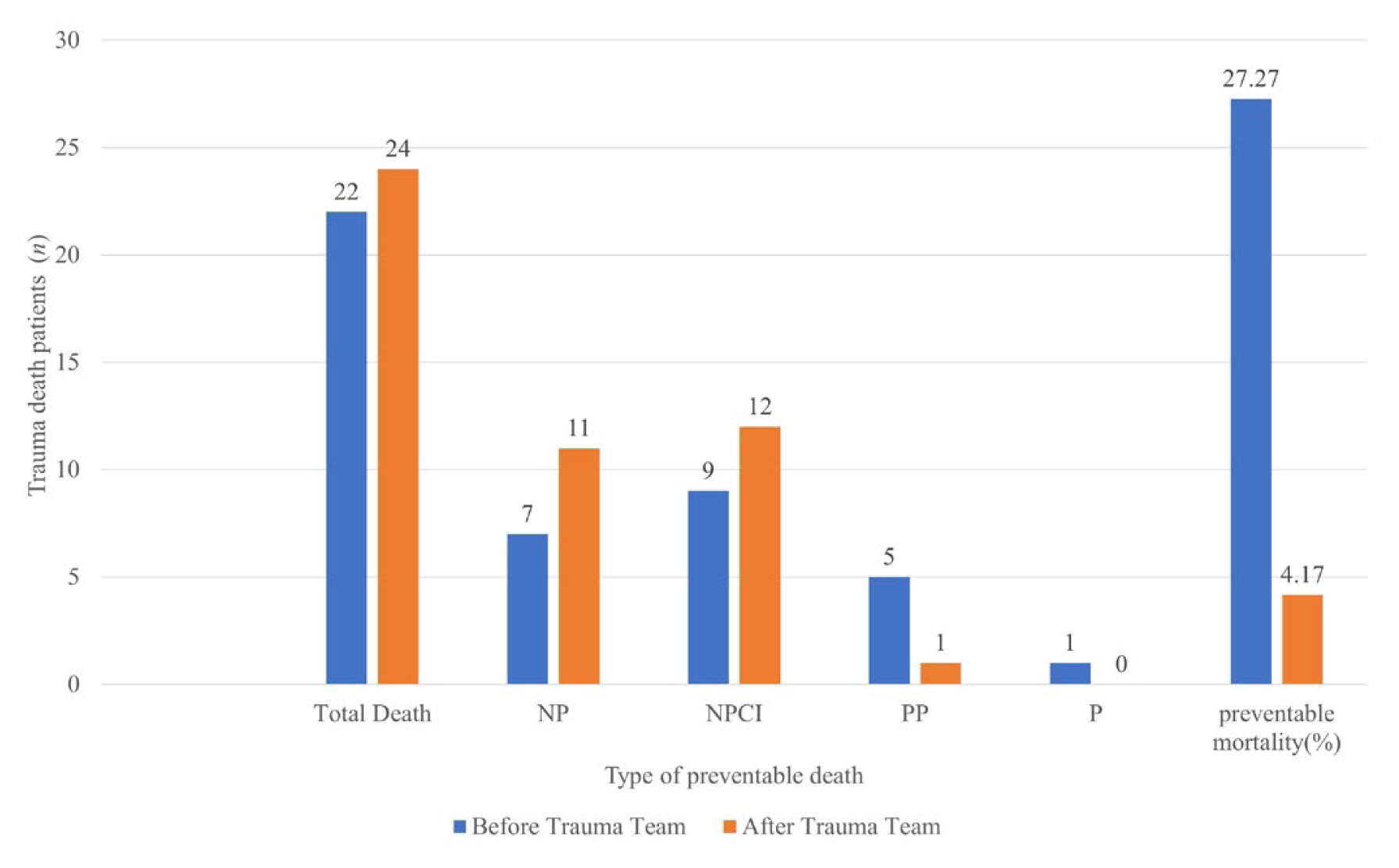
Comparing before and after implementing the Trauma Team. NP = non preventable; NPCI = non preventable but with care that could have been improved; P = preventable; PP = possibly preventable.
Discussion
In this retrospective study TBI was the leading cause of traumatic mortality, accounting for 39% of deaths however, no preventable or possibly preventable deaths occurred. The 2nd most frequent death was respiratory arrest which was the 2nd common cause for preventable death. Prolonged care of immobilized patients in the Intensive Care Unit or on the ward caused pneumonia and respiratory failure, and inadequate treatment with antibiotics and line infection were the causes. The 3rd most common cause of death was due to bleeding. The most common errors in death caused by bleeding were delayed damage control surgery and delayed transfusion. Based on the general domestic regional trauma center preventable mortality audit criteria, the definition used for delayed time for damage control surgery was the time taken from trauma to admission of the patient to the operation theater to be over one hour and delayed transfusion was defined as when the time from ER arrival to the first transfusion was more than 30 minutes [4,11]. The proportion of causes of death of patients with trauma evaluated in this study was similar to other research [12]. The preventable death rate significantly decreased from 27.27% to 4.17% after the Trauma Team was initiated (p = 0.021).
The most common errors can be reduced by ensuring quality control in the hospital for example is reducing the time waiting for the patient to receive a transfusion, checking the timing of DVT prophylaxis, and ensuring adequate management of IV-lines. The Emergency Department doctors are highly trained in the primary survey (ABCDE), but do not have time or enough staff to enable them to dedicate their resources exclusively to trauma patients. Therefore, they might miss the timing of transfusion when a patient is in ATLS Class II or III when systolic blood pressure does not drop. Trauma surgeons recognized this error and a system to give transfusion as quickly as possible was developed for patients in need [13]. Prolonged care in the Intensive Care Unit, and immobilized trauma patients are at risk of developing DVT, and this should not be underestimated. Chemoprophylaxis is recommended within 48 hours of trauma, in some guidelines chemoprophylaxis must be administered within 24 hours but it is not easy to start chemoprophylaxis due to ongoing bleeding or rebleeding after chemoprophylaxis, especially in TBI patients [14–16]. Management of IV-line error occurred when hemodynamically unstable patients did not have 2 large bore needles at the antecubital fossa in accordance with ATLS recommendations, or central lines inserted in the femoral vein were not removed within 48 hours which can increase the risk of DVT and central line infections if not removed immediately when noticed. After the Trauma Team trained the ER nurses on accurate peripheral IV-line administration, these errors were reduced.
In Gyeonggi province the preventable death rate in 2017 was 17% [5]. In 2021, a single center regional trauma center preventable death rate was 8% [12]. In this current study the PDTR was 22.4% overall and 4.17% after the Trauma Team was initiated. The average PTDR in a non-regional trauma center in a general tertiary hospital larger than 500 beds was 30.7% in 2015 and the PTDR of a non-regional trauma center varied from 12.9% to 23.7% in 2019 [2,3]. The PTDR of the NHISIH before the Trauma Team was initiated was 27.3% which was similar to the national data. The PTDR dropped statistically significantly to 4.17% after the Trauma Team was initiated (p = 0.021). There are a few reasons that have led to this decrease. Firstly, co-management with the Emergency Department has led to fewer errors. Secondly, consistent education of health workers related to treating trauma patients. Thirdly, an active leadership by trauma surgeons in managing multiple trauma patients has led to a reduced waiting time for trauma patients that were treated in the ER by staff other than Emergency Department doctors. This decrease in PTDR shows the Trauma Team with a trauma specialist could reduce preventable deaths in non-regional trauma center hospitals.
The PTDR of a regional trauma center can be reduced by addressing in-hospital errors and prehospital errors. In-hospital death rates have been reduced but there is room for improvement in prehospital errors. A trauma patient has a much higher chance of preventable trauma death when transferred or arrives at a treatable hospital within the hour [2]. A hospital like the NHISIH, with a trauma surgeon can help reduce the pre-hospital errors of a regional trauma center by training staff to perform resuscitation that can buy time for a patient before being treated in a regional trauma center or at a local hospital.
There are limitations to the study. Firstly, it was a retrospective single center study and the trauma patient pool was smaller and less representative than other trauma centers. Secondly, the severity of trauma may bias the results in this study. Finally, the reviewers were all from General Surgery and Trauma Departments and may have caused a bias in results for organ injuries especially traumatic brain injury.
There are national data for PTDR and mortality at institutions other than regional trauma centers [2,3,6]. The strength of this study was that it provided domestic data of how a Trauma Team that can significantly improve the PTDR of a local emergency center.
Conclusion
The implementation of a Trauma Team significantly reduced the PTDR of a non-regional trauma center. Running a dedicated Trauma Team in a hospital other than a regional trauma center, reduced the incidence of medical errors that can be caused when treating trauma patients.
Notes
Author Contributions
Conceptualization: JYJ. Methodology: JYJ, KP, and SL. Formal investigation: KP, SL, and KYL. Data analysis: KP, SL, KYL, DC, and HY. Writing original draft: KP and WRC. Writing - review and editing: KP and JYJ.
Conflicts of Interest
Ji Young Jang has been the associate editor of Journal of Acute Care Surgery since January 2017, but had no role in the decision to publish this original article. No other potential conflict of interest relevant to this article was reported.
Funding
This work was supported by a National Health Insurance Service Ilsan Hospital grant (no.: NHIMC-2022-CR-037).
Ethical Statement
Ethical approval was obtained from the Institutional Review Board of the NHISIH (IRB no.: 2022-3-022-001).
Data Availability
All relevant data are included in this manuscript.