Deep Neck Infection with Mediastinal Abscess Treated by Modified Vacuum-Assisted Closure Application
Article information
Abstract
Deep neck infection is a surgical emergency that can result in life threatening complications such as airway obstruction, aspiration, thrombosis of major vessels and mediastinitis by spread of infection along fascial planes. Although appropriate surgical intervention and prompt antibiotics are given, revision surgeries are often required. We report a patient with mediastinal abscess caused by a deep neck infection that was initially intractable with usual surgical drainage but was eventually successfully treated with the modified application of a vacuum-assisted closure (VAC) device (InfoV.A.C. Therapy Unit; Kinetic Concept Inc., USA). We inserted silastic drain tubes into paratracheal area. It was difficult to pack the VAC foams, so they were prone to fail, with complete debridement. With modified VAC therapy assisted by silastic drain tube, the deeply located mediastinal abscess that had been unresponsive to conventional surgical drainage was successfully treated.
Introduction
Several important visceral structures such as esophagus, trachea, thyroid gland, vessels, and spines, etc. are located within the deep neck space. Those organs are bound together by loose connective tissue and intercommunicate to varied degree, which facilitates a single infection within the space to spread rapidly to adjacent space. The anatomical feature allows an infection in the space between alar and prevertebral fascia to drain into the posterior mediastinum by gravity, resulting in mediastinitis and empyema. Once an infection extends to mediastinum, the mortality reaches 40∼50% [1] and repeated operations are not uncommonly required due to its inaccessibility [2].
We report our experience with a patient of mediastinal abscess caused by deep neck infection from decayed teeth which was initially intractable after 2 times of incision and drainage, but was eventually successfully treated with the modified application of a vacuum-assisted closure (VAC) device. To our best knowledge, it is the first report to describe the application of additional tube insertion underneath the VAC foams in a mediastinal abscess.
Case Report
A 26-year-old male who didn’t have any underlying diseases visited the emergency room at a university hospital with fever, pleuritic chest pain, and hemoptysis that began 2 days ago. He underwent dental procedures for tooth decay a month ago and had been drinking excessively since two weeks before the admission.
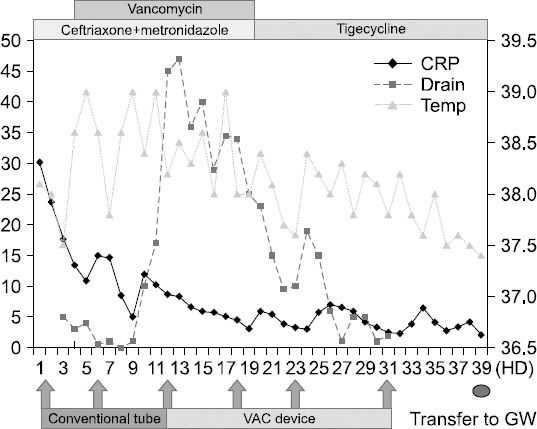
On admission, his vital signs were as follows: blood pressure 132/76 mmHg, pulse rate 102/min, respiratory rate 18/min, and body temperature 38.1°C. On physical examination, his mental status was clear, but diffuse swelling and tenderness were observed over the whole neck area without definitive erythematous change or heating sense. The initial complete blood count was as follows: leukocytes 20,600/mm3 (neutrophils 82%, band form 8%), hemoglobin 16.2 g/dl, and platelets 173,000/mm3. His initial blood chemistry was as follows: blood urea nitrogen 42.4 mg/dl, creatinine 2.63 mg/dl, aspartate transaminase 38 U/L, alanine transaminase 20 U/L, alkaline phospatase 42 U/L, total bilirubin 3.35 mg/dl, lactate dehydrogenase 278 U/L, creatine phosphokinase 458 U/L, and C-reactive protein (CRP) 30.15 mg/dl. Chest X-ray and low radiation high resolution chest computed tomography (CT) showed a upper mediastinal widening (Fig. 1A). Third generation cephalosporin (ceftriaxone) plus metronidazole were started in order to cover potential deep neck infection, then he was admitted to a general ward.
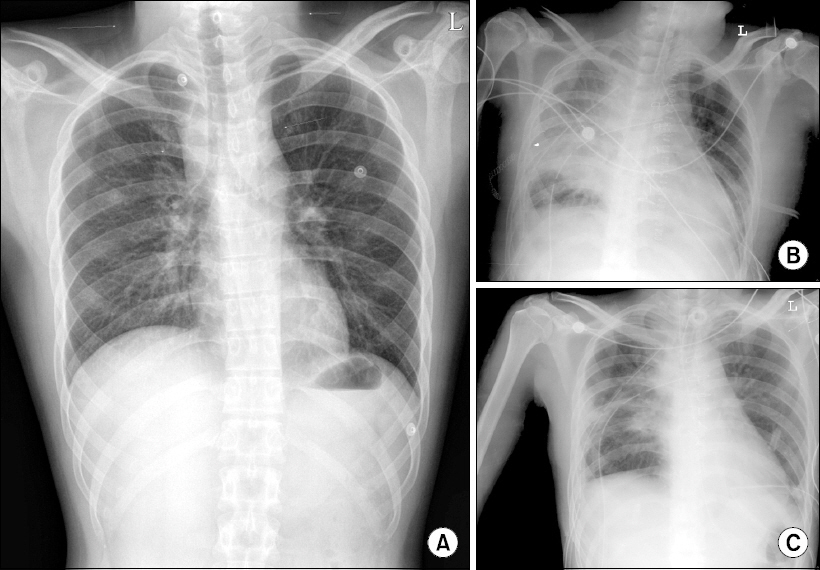
Chest radiograph images were obtained on hospital day 1 (A), 12 (B), and 31 (C). (A) Chest X-ray on admission showed a widening of superior mediastinum. (B) On hospital day 12, newly development of right lung abscess was observed. (C) On hospital day 31, a remarkable improvement was achieved.
On hospital day 2, hoarseness, dyspnea, and rapid progression of swelling and erythema on whole neck area were observed. Neck CT with enhancement showed retropharyngeal fluid collection spreading to mediastinum (Fig. 2A). Subsequently, intubation and emergency surgical drainage were performed. Through a cervical and sternal incision, a large volume of purulent secretions was drained. After abundant curettage of necrotic tissue with massive saline irrigation, a conventional drain tube was placed into the mediastinum. Total amount of daily pus drainage through mediastinum was less than 50 ml. Samples of purulent secretions were collected during the operation and sent to microbiological laboratory. Bacteroides spp. Streptococcus constellatus and methicillin-resistant Staphylococcus epidermidis were detected at the microbiological culture. We added vancomycin accordingly.

Chest computed tomography (CT) images were obtained on hospital day 2 (A), 12 (B), 16 (C), and 31 (D). (A) Chest CT on hospital day 2 showed abscess formation in the superior mediastinum. (B) The day before a vacuum-associated closure (VAC) device placement, progression of mediastinal abscess with newly developed abscess formation on right upper lung zone was observed. (C) After 4 days from a VAC device placement, remained complicated fluid collection and the silastic tube (arrow) underneath the VAC foam were observed. (D) After 19 days from a VAC device placement, a remarkably decreased amount of abscess was observed.
On hospital day 6, significant rebound of inflammatory markers (leukocyte 31,440/mm3, CRP 14.97 mg/dl) and sustained fever (up to 38.6°C) were observed. At the follow-up CT, cervical abscess pockets were shrinked; however, significantly increased amount of mediastinal abscess was found. With those findings, we performed additional surgical drainage with drain tube insertion same as that of hospital day 2. Less than 10 ml of daily pus drainage through mediastinal drain tube was achieved thereafter.
On hospital day 12, mediastinal abscess pockets were augmented and pulmonary abscess was newly developed at the follow-up chest X-ray and CT (Fig. 1B, 2B). Another surgical debridement and massive saline irrigation was done followed by a VAC device (InfoV.A.C. Therapy Unit; Kinetic Concept Inc., San Antonio, TX, USA) placement over mediastinal wound instead of conventional tube insertion. A silastic drain tube was inserted into paratracheal area where abscess pocket was located, positioning opening side upward in order to attach to the lower surface of VAC foams (Fig. 2C). Then VAC foams carefully placed to fill the anterior mediastinal cavity underneath the sternotomy site. The wound was tightly draped with transparent film to avoid air leakage. The VAC device was connected to the VAC foams and set to provide a continuous pressure of -125 mmHg.
Thereafter, significantly increased amount of daily pus drainage through mediatinal wound was observed. Accordingly, his vital signs became stabilized and inflammatory markers began to improve (Fig. 3). Further surgical drainages with exchange of VAC foams were done on hospital day 18 and 23, respectively. Multi-drug resistant Acinetobacter baumanii was found at the follow-up pus culture which was obtained during the operation of hospital day 23, thus, we changed antibiotics to tigecycline. Daily pus drainage through mediastinal wound gradually decreased over time, and no more residual pus was observed at the mediastinum in follow-up X-ray and CT on hospital day 31 (Fig. 1C, 2D). Consequently, the VAC device was removed and the sternal incision site was closed. During the procedure, we can confirm the successful toileting and healing of the deep tissues. The patient was transferred to a general ward on hospital day 39. Finally the patient was discharged on hospital day 73.
Discussion
In addition to the proper antimicrobial therapy, surgical drainage is imperative in most deep neck infections, especially in complicated cases: presence of airway impairment, descending infection, and involvement of major vessels, etc. [3]. Drainage tubes are routinely placed into the infected area after irrigation and debridement in order to remove remained secretions and prevent pus collection [4]. However, the adequate drainage is hard to be achieved in deeply located wounds such as mediastinal abscess.
The negative pressure therapy with a VAC device was first introduced to clinical field in 1997 and has been utilized continuously in several intractable wounds [5]. Negative pressure promotes removal of exudates and reduction of edema, allowing enhancement of granulation tissue formation and increase tissue perfusion. Moreover, larger wound surfaces can be covered [4], and microbe removal is boosted by negative pressure [6]. Despite the absence of large scale study, negative pressure therapy is thought to be effective in mediastinal abscess [7]. Indeed, the method has been gradually gaining acceptance for the management of mediastinal infection [7-9]. However, mediastinal abscess still remains one of the most difficult wound to be drained and treated well. A study in Netherlands showed a 12.5% of in-hospital mortality rate and a 28% of treatment failure rate in patients with post-sternotomy mediastinitis treated by a VAC device [10]. If abscess pockets are located deeply in the mediastinum, the adequate wound packing by VAC foams is hard to be achieved and it may lead to treatment failure.
The remarkable point in this case is that silastic tube insertion underneath the VAC foam. In order to facilitate drainage, we inserted additional tube into the abscess pocket, applying VAC foams over the opening site of the tube. Consequently, a significant large amount of pus was drained, which led to treatment success.
We report a patient of intractable mediastinal abscess caused by deep neck infection who was successfully treated with the modified application of a VAC device. Although further studies are needed to evaluate the efficacy of our procedure, we suggest additional silastic tube insertion underneath the VAC device can be an effective option for treatment of intractable mediastinal abscess.
References
Notes
Conflicts of Interest
No potential conflict of interest relevant to this article was reported.