Delayed Splenic Pseudoaneurysm Formation after Angioembolization
Article information
Body
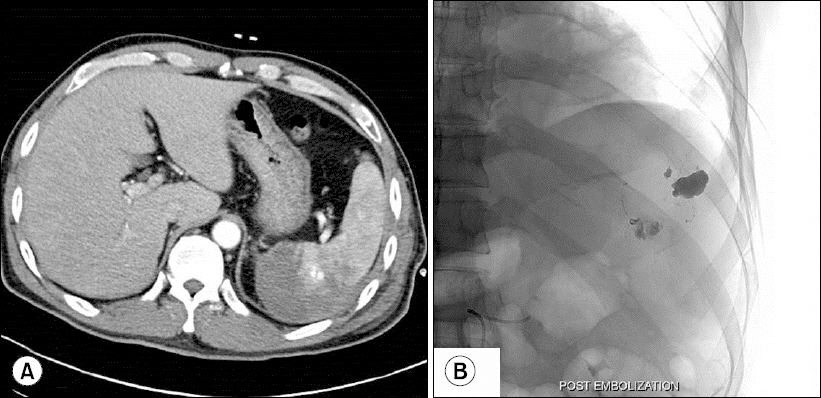
A 48-year-old man experienced blunt abdominal trauma after falling from a height of 7 meters. His systolic blood pressure upon arrival was 120 mmHg, and heart rate was 95 beats per min. Abdominal computed tomography (CT) upon admission revealed contrast leakage from a splenic injury (grade 3) (Fig. 1A). Emergency angiography and embolization were performed using gelfoam (Fig. 1B). CT, repeated 7 days after his trauma revealed a pseudoaneurysm (Fig. 2A). Angioembolization was performed to prevent bleeding from the pseudoaneurysm (Fig. 2B). CT performed a week later revealed no pseudoaneurysm. The patient recovered well and was discharged home There is a lack of evidence regarding the optimal period/frequency of performing CT follow-up after angioembolization for splenic injuries [1,2]. Our present case indicates that close follow-up including CT is warranted in patients undergoing angioembolization to monitor for delayed pseudoaneurysm formation.

Computed tomography scan and angiographic images obtained upon admission: (A) Perisplenic contrast blush can be observed. (B) Embolization was performed using gelfoam.
Conflicts of Interest
No potential conflict of interest relevant to this article was reported.
References
Notes
Conflicts of Interest
No potential conflict of interest relevant to this article was reported.