Introduction
Surgical conditions represent about 30% of the global burden of diseases [
1]. The disease control priority project estimates that 11% of all the disability adjusted life years lost globally are from surgical conditions [
2]. In 2010, there were 896,000 deaths, 20 million years of life lost, and 25 million disability adjusted life years lost from only 11 emergency general surgical conditions, with 70% of deaths occurring in low- and middle-income countries [
1]. The burden continues to rise steadily, disproportionately affecting low- and middle-income countries as many move through the epidemiologic transition away from communicable diseases towards non-communicable diseases [
3]. Emergency surgeries carry a disproportionate burden of risk for medical errors, complications, and deaths compared with elective procedures [
4]. Abdominal surgical emergencies contribute substantially to the burden of these surgical emergencies and are associated with a high risk of postoperative morbidity and mortality [
5,
6]. In Nigeria abdominal surgical emergencies accounted for approximately 29.5% of all emergency surgical admissions [
7].
The indications and outcomes of emergency abdominal surgery vary within different settings from high, middle to low-income countries [
8]. A study in Russia revealed acute appendicitis, acute cholecystitis, and acute pancreatitis as the most common abdominal surgical emergencies [
9]. A similar study in the USA, showed peptic ulcers and small bowel obstruction due to adhesions as the most common indications for emergency abdominal surgery [
8]. In Africa, a 2-year study carried out in Ethiopia showed that intestinal obstruction, acute appendicitis, and bowel perforation were the leading causes of abdominal surgical emergency admissions [
10]. A similar pattern was reported in a study from Ghana [
11]. In Cameroon in 2019, the most common abdominal surgical emergencies were intestinal obstruction, acute appendicitis, peritonitis, and trauma [
12]. Management of surgical emergencies remains a challenge in resource limited settings because delayed presentation of patients requiring surgery is common, which is mainly due to the transfer of patients between facilities among other factors [
13,
14]. Emergency abdominal surgery is generally associated with a high post-operative mortality [
2,
5,
8,
13]. The United Kingdom (UK) Emergency Laparotomy Network and the American College of Surgeons National Surgical Quality Improvement Program reported 30-day mortality after emergency abdominal surgeries as 14.9% and 14%, respectively [
13,
15]. In Africa mortality is higher (16.6% in a study in Malawi and 18% in Ghana) [
11,
16]. Although many studies have been carried out on abdominal surgical emergencies, there is need to update our knowledge as patterns change over time. In this retrospective study, we aimed to review the indications for emergency abdominal surgery, determine the delay in presentation, describe the outcomes after surgery, and identify the factors associated with mortality in Cameroon.
Discussion
In this study, we aimed to review the spectrum, management, outcomes of abdominal surgical emergencies, and the factors associated with postoperative mortality in a referral hospital in a middle-income country in Sub-Saharan Africa.
Abdominal surgical emergencies affect a heterogeneous group of people including all age groups and genders. Male predominance (male to female ratio = 1.4:1) was observed in this study which is in agreement with other studies in Africa, and even in the developed world [
12,
13,
18,
19]. The mean age was 47.4 years which is comparable with findings in South Africa reported by Rickard et al [
8], in the USA reported by Purcell et al in Malawi [
16]. However, this age is much older than findings from other studies in Africa [
10,
11,
20]. This is probably because these studies included pediatric populations. Abdominal surgical emergencies in this review were determined to be highest in the 3rd and 4th decades of life which is in agreement with other studies in Africa. [
10,
11,
21]. However, Saunders et al [
13] in the UK reported highest frequencies in the 6th and 7th decades of life.
Intestinal obstruction, perforated peptic ulcers, acute appendicitis, ruptured ectopic pregnancies, and acute cholecystitis were the most frequent abdominal surgical emergencies in this study. Engbang et al [
12] reported similar findings in Douala, Cameroon. These findings are also similar to studies from other African countries that reported intestinal obstruction as the most common abdominal surgical emergencies [
10,
11,
16,
22,
23]. These findings are different from that reported by Ahmed et al [
7] in Zaria and Nigeria, and findings by Kotiso et al [
21] in Ethiopia who demonstrated acute appendicitis as the commonest abdominal surgical emergency. In developed countries, reports from Russia and the USA show acute appendicitis and peptic ulcers, respectively, as the most common abdominal surgical emergency [
8,
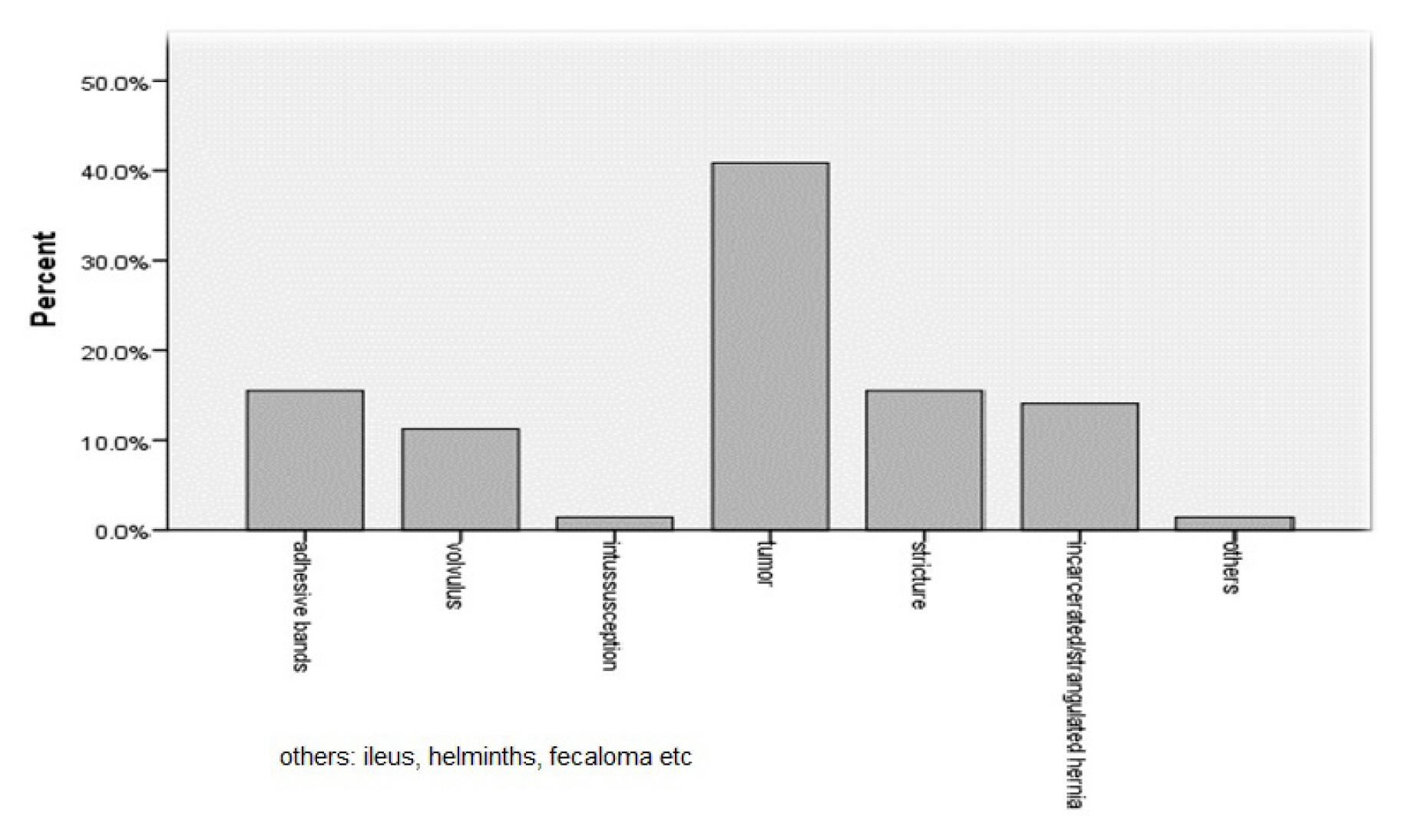
9]. Although, like in most Sub-Saharan African countries, intestinal obstruction is the most common cause of abdominal emergencies, in this study, its etiology is mostly tumors (40.8%), adhesive bands (15.5%), incarcerated / strangulated hernias (14.1%), strictures (15.5%), volvulus (11.3%), and intussusception (0.5%). This is in contrast to many studies in Africa that have reported incarcerated hernias and volvulus as the most frequent cause of intestinal obstruction [
7,
10]. The higher incidence of tumor-related intestinal obstruction may be because this hospital is a referral hospital for the region and the only hospital with a medical oncologist in the northwest region. Therefore, it has many patients who are referred with primary colon cancers and metastasis of other cancers causing bowel obstruction. Despite this, more studies need to be carried out to understand the high frequency of tumor-related intestinal obstruction in this setting. The higher frequency of adhesive bands is similar to reports from Ethiopia [
21]. However, in Nigeria, a changing pattern of intestinal obstruction has been reported. Strangulated hernias were the most frequent cause of bowel obstruction, however, adhesions have become the most dominant cause [
20]. Furthermore, the frequency of typhoid ileal perforation was determined in this review to be much lower than reports from other African countries [
7,
11]. This may represent success in prevention and early treatment of typhoid in our setting, or may be due to the extensive use of antibiotics.
More than 50% (62.8%) of the patients were referred from other health facilities. This is in accordance with several studies carried out at teaching hospitals in Africa [
16,
17–
19]. The median delay from onset of symptoms to presentation was 6 days, with minimum and maximum delays of 28 minutes and 21 days, respectively. This is in agreement with a study performed in Ethiopia where the average duration from the onset of symptoms to admission was 5 days (ranging from 6 hours to 21 days), and a study by Chao Long et al performed at Mbingo Baptist Hospital where 60.3% of patients presented more than 7 days after onset of symptoms [
19,
21]. However, this is much higher than reported by Berhanu Nega et al on a study in Ethiopia [
10]. This long delay in presentation in our setting is probably due to the low socio-economic status of the patients and hence the tendency of patients to try alternative medicines first and consult only after its failure. These delays in the diagnosis and referral from lower-level health facilities are probably because the majority of the population must consult these health centers first, then be referred to the district hospitals, before admitted to the referral hospital. The in-hospital delay from presentation to surgery was 8 hours (median). This compares favorably with other studies from Africa [
12,
22]. However, this is still very high when compared with findings from developed countries. This long in-hospital delay in our setting may be due to time spent in reanimation / resuscitation of the patient before surgery. In the absence of a health insurance system or universal healthcare coverage, most patients must pay for surgical and resuscitation services which delays the procedure as patients try to gather funds.
An emergency laparotomy was carried out in 94.3% of cases and a laparoscopy in 5.3%. In this study, the average length of hospital stay after surgery was 11.7 days, which falls within the 7 to 12 days average range reported in some Sub-Saharan countries after emergency abdominal surgeries, even though this depends on the setting and characteristics of the study population [
7,
16,
18,
19]. In our study, 100 (48.3%) patients developed a complication and 72 (34.7%) had a major complication (Clavien Dindo > 3). This is comparable to a report in the UK by Howes et al where almost all patients (97%) experienced at least a postoperative morbidity survey (POMS) - defined morbidity after emergency abdominal surgery [
24]. A higher percentage was reported by Tengberg et al in a study in Denmark where 71% of the patients had at least one complication and 47% had a major complication (Clavien Dindo ≥ 3) [
25]. However, our findings are much higher than a study in Ethiopia where 20% of the patients had at least one complication [
21]. High complication rates are understandable since emergency abdominal surgery is high risk surgery and patients almost always present with some physiological derangements especially in patients that present late to the hospital. The lower rates of complications in Ethiopia are probably because patients presented earlier to the hospital (average of 4.6 days as compared to 6 days in our study) and were younger (mean of 28 years as compared to 47 years in our study). Surgical site infection followed by sepsis, anemia, and acute kidney injury were the most frequent complications observed in our study. This is similar to findings from other studies [
22,
24].
Emergency abdominal surgery in Africa is associated with high mortality rates ranging from 5.4% to 23.1% [
7,
8,
13,
16,
18,
19,
21,
24]; we observed a mortality of 19.8% in this review which is within this range, and is comparable to 18% and 19.4% reported by Nyundo et al [
18] and Clarke et al [
26] in Rwanda, and the UK, respectively. Even though the mortality rate in this review falls within the range in most Sub-Saharan countries, the rates observed are higher than some reports from Africa and developed countries [
7,
8,
15,
16,
21]. This is probably because our patients were older (mean age 47.4 years) and had longer delays from onset of symptoms to presentation at the hospital (6 days).
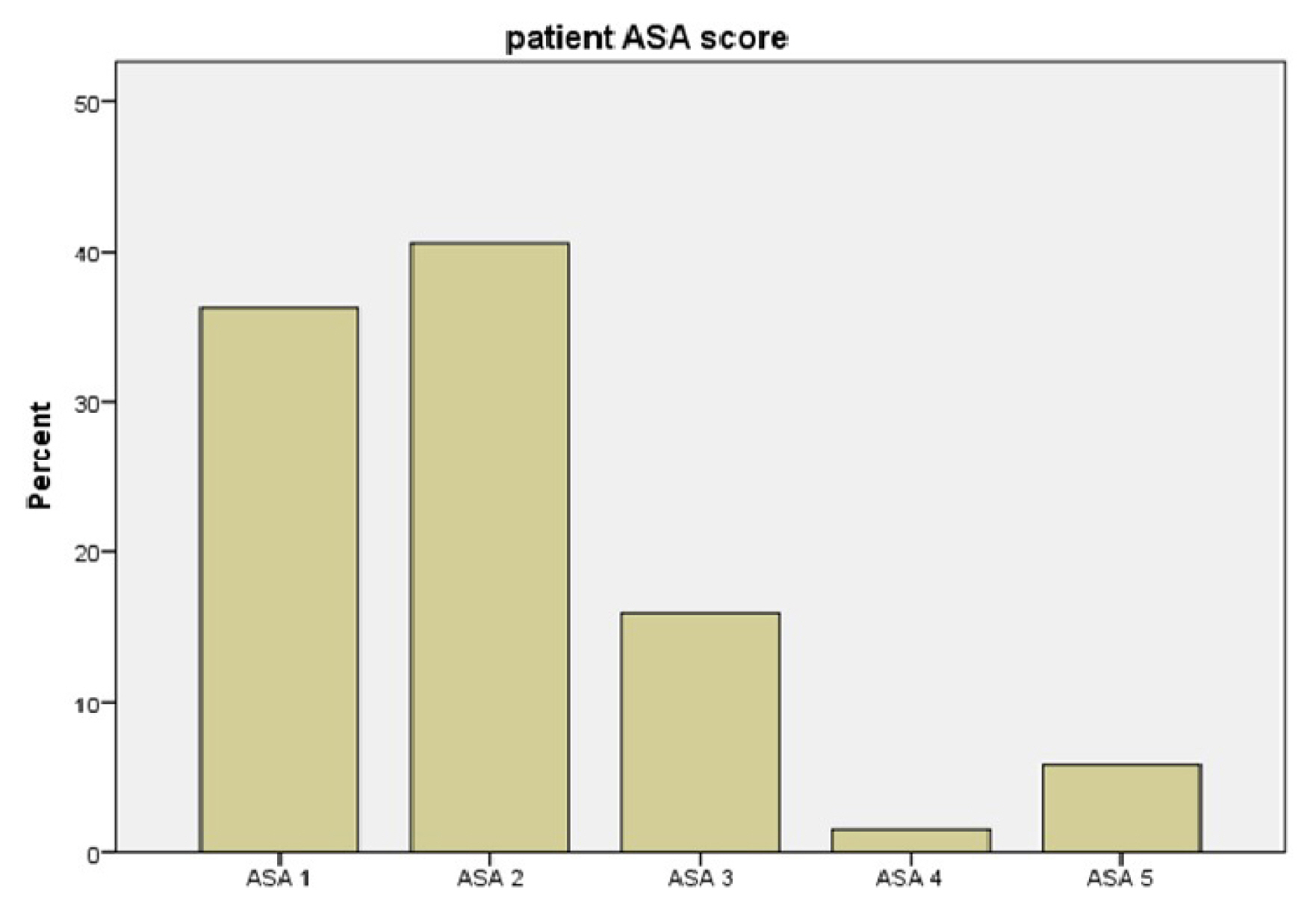
Several factors are associated with mortality in emergency abdominal surgery. Recognition of these factors in our setting is important in order to guide efforts aimed at better management and improving outcomes. We determined that, mortality was independently associated with a high ASA score (ASA > 3), age > 60, referral from other health facilities, and other diagnoses including ruptured aortic aneurysms, retroperitoneal gangrene, and necrotizing fasciitis. This is in agreement with studies in both Africa and developed countries which all observed high ASA scores and age as independent risk factors for mortality [
8,
16,
21]. The absence of reanimation facilities and key cardiopulmonary monitoring may be responsible for this mortality. In addition, many studies in Sub-Saharan Africa have reported increased mortality in patients referred from other health facilities as observed in this study [
15,
17]. This is probably due to delays in management and physiological derangements. Patients are being transferred from one hospital to another (which usually amounts to being admitted to several hospitals before arriving at Mbingo Baptist Hospital). In addition, the use of non-medicalized means of transportation of patients from one health facility to another may affect mortality rates; and this reflects some health care limitations in Cameroon. The association of mortality and referral from other health facilities in Sub-Saharan Africa reflects the limited accessibility to timely care in these countries. Contrary to studies that report comorbidities, delays to surgery, and some diagnoses like peptic ulcers, and typhoid ileal perforation, we observed no statistically significant association between mortality and these factors [
8,
14,
16,
18]. More studies need to be carried out to understand these differences.
The study is limited based on its retrospective nature and as such, these findings may not be representative of the population. In addition, we used deaths recorded in the hospital for 30 days postoperative mortality; this may not represent the true mortality as this did not include those patients who died after discharge. The retrospective nature of the study coupled with the limited infrastructure in the hospital, which is representative of most peripheral referral hospitals in Africa, limits the evaluation of some important respiratory and physiological parameters. This limited the use of validated systems such as the sequential organ failure assessment scores and acute physiology and chronic health evaluation 2 scores which would otherwise provide valuable entities and parameters to evaluate the factors related to mortality. As such, other important entities such as transfusion, vasopressor use, duration of antibiotic-therapy, nutrition, and other factors which have a huge potential to influence the morbidity and mortality could not be evaluated completely.
It is imperative to carry out a multicenter prospective study to better understand the true etiology of intestinal obstruction. This study was carried out at the only cancer treatment facility in the region, this may explain the high number of tumor-related intestinal obstructions, and the true incidence of peritonitis secondary to typhoid perforation in Sub-Saharan Africa.