|
 |
- Search
| J Acute Care Surg > Volume 13(1); 2023 > Article |
|
Abstract
Purpose
Renal injury occurs in up to 5% of trauma cases and the kidney is the third most wounded abdominal organ. The study objective was to analyze clinical characteristics of patients with blunt renal trauma and review the treatment of high-grade blunt renal injuries.
Methods
The medical charts of trauma patients who visited Haeundae Paik Hospital between March 2010 and February 2020 were retrospectively analyzed. Data on demographics, injury patterns, clinical presentation, management, and outcomes were analyzed.
Results
A total of 68 patients with renal trauma were included in this study. The most common renal injury was Grade III (n = 27, 39.7%). Falling was the predominant mechanism of injury (n = 33, 48.5%), and 23.5% (n = 16) of patients sustained isolated renal trauma. Organ damage related to kidney injury included chest injury (57.4%, n = 39) and abdominal or pelvic content injury (48.5%, n = 33). The overall mortality rate was 2.9% (n = 2). There were 45 cases of high-grade renal trauma (AAST Kidney injury scale Grade IIIŌĆōV). There was no statistical difference in the outcomes of high-grade (n = 44, 97.8%) and low-grade (n = 23, 100%) renal trauma patients who received nonoperative treatment (p = 0.511). Variables did not differ significantly, except for the injury severity score which was statistically significantly different between low-grade and high-grade renal trauma patients (p = 0.001).
Anatomically, the kidneys are well-protected by strong lumbar muscles, vertebrae, ribs, and abdominal viscera on the anterior side. However, these genitourinary organs are most often injured as a result of blunt trauma [1]. Renal injury occurs in up to 5% of all trauma cases and the kidney is the 3rd most wounded solid abdominal organ [2ŌĆō5]. The ultimate goal of kidney-injury treatment is to save the patientŌĆÖs life by controlling bleeding, preserving nephron function (as much as possible), and minimizing the risk of related complications. In the past, the common practice for achieving these goals was surgery. Recently, nonoperative management has been proposed as a standard treatment method for patients with low-grade blunt renal injury [4ŌĆō6]. This shift was driven by the accrued knowledge over the last 3 decades on the safety and outcome of nonoperative management, with advances in imaging and embolization techniques, and in minimally invasive treatment techniques such as ureteral stenting [7ŌĆō10]. In addition, the treatment of patients with high-grade renal injury has also been shifting from surgery to nonsurgical treatments [6ŌĆō8].
The guidelines of the World Society of Emergency Surgery (WSES) and the American Association for the Surgery of Trauma (AAST) recommend nonoperative management, which may include angioembolization, if vital signs are stable, regardless of the AAST Kidney injury scale [3]. While surgical treatment is recommended for patients who are hemodynamically unstable and not responsive to fluid resuscitation, the WSES-AAST guidelines suggest that nonoperative management should always be considered as the first option whenever possible [3].
Compared with trauma centers (with specialized teams and equipment to handle serious trauma), non-trauma centers have limitations in following the WSES guidelines in the treatment of renal injury patients due to the lack of resources and expertise.
The objective of this study was to review cases of blunt renal injury at a non-trauma center, analyze the clinical features and outcomes of patients, and consider the care of high-grade blunt renal injury patients.
This retrospective study was approved by the institutional review board of Haeundae Paik Hospital (no.: HPIRB 2021-10-009). The clinical data of patients who presented in the Emergency Department (ED) with blunt abdominal injury between March 2010 and December 2020 were identified from electronic patient records. The inclusion criteria were patients aged > 18 years who were admitted to the Emergency Department with blunt abdominal trauma. Patients excluded from the study: Ōēż 18 years, suspected renal trauma but without computed tomography (CT)-verification, died in the Emergency Department, or had renal trauma (ureter or bladder).
Data collected included age, sex, mechanism of injury, renal injury grade according to the AAST Organ injury scale, injury severity score (ISS), heart rate, systolic blood pressure, laboratory data including hemoglobin levels (particularly the lowest level recorded during the first 24 hours), other associated injuries, transfusion within two days of hospitalization, treatment options, length of stay (LOS) in the intensive care unit, LOS in the hospital, and mortality. All patients underwent contrast-enhanced CT at the time of ER admission. Renal injury was diagnosed using CT and was classified according to the AAST Kidney injury scale. Patients with renal injury were grouped as low-grade injury (AAST Grade I and II), or high-grade injury (AAST Grade III to V) based on the 2018 AAST Organ injury scale [11].
The Kolmogorov-┬¼Smirnov test was performed on the data to verify the assumption of normality. Categorical data were reported as numbers and percentages, whereas continuous data were reported as the median and interquartile range. Categorical variables were compared using the Chi-square or FisherŌĆÖs exact tests, whereas continuous variables were compared using the Mann-Whitney U test. All statistical analyses were performed using MedCalc software (MedCalc Software Ltd., Ostend, Belgium). Differences were considered significant if the two-tailed p value was < 0.05.
A total of 92 trauma patients with kidney injury presented at the ER of Haeundae Paik Hospital between March 2010 and February 2020. Based upon the study inclusion criteria, 24 patients were excluded, and the data of the remaining 68 patients were analyzed.
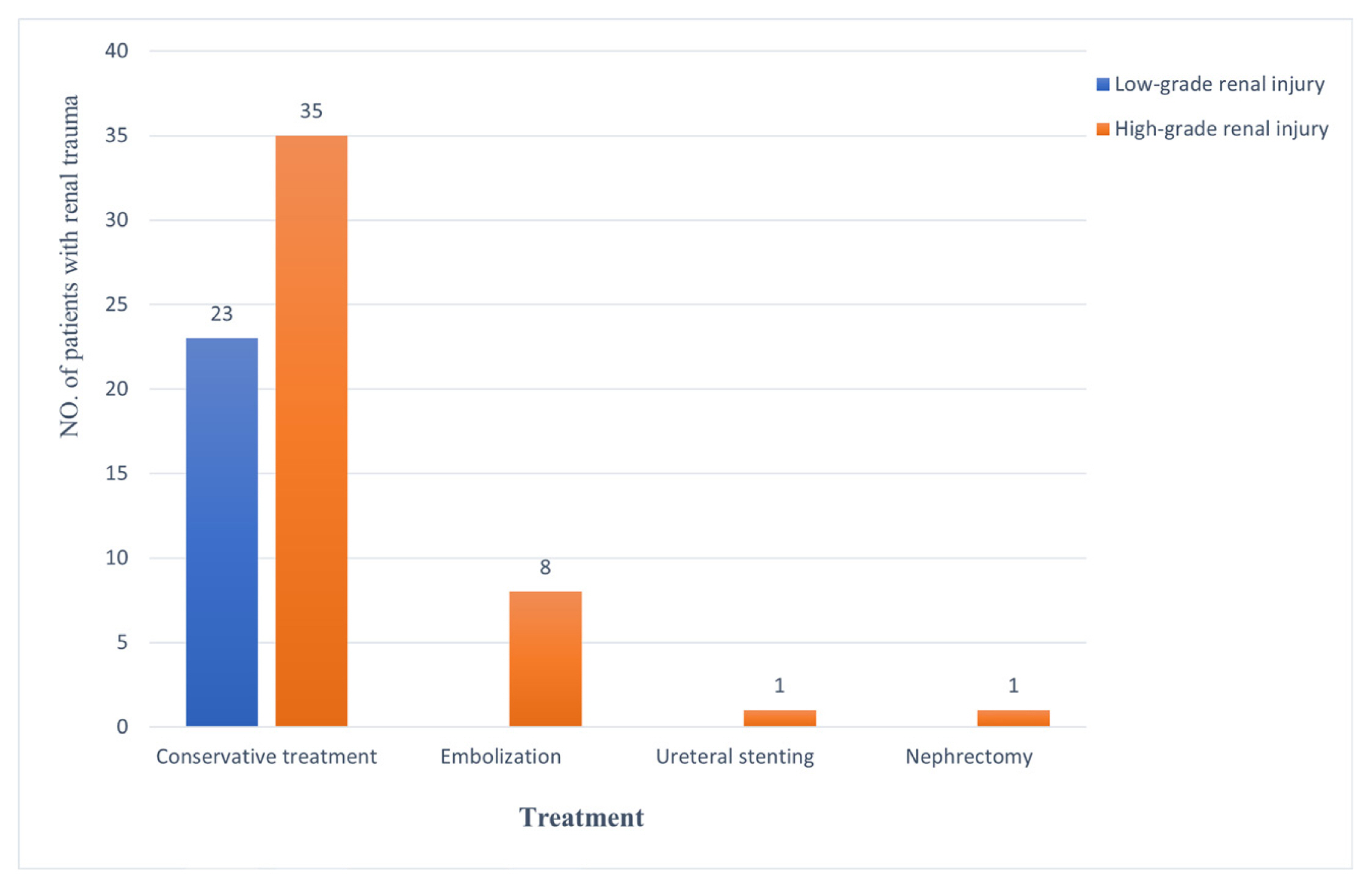
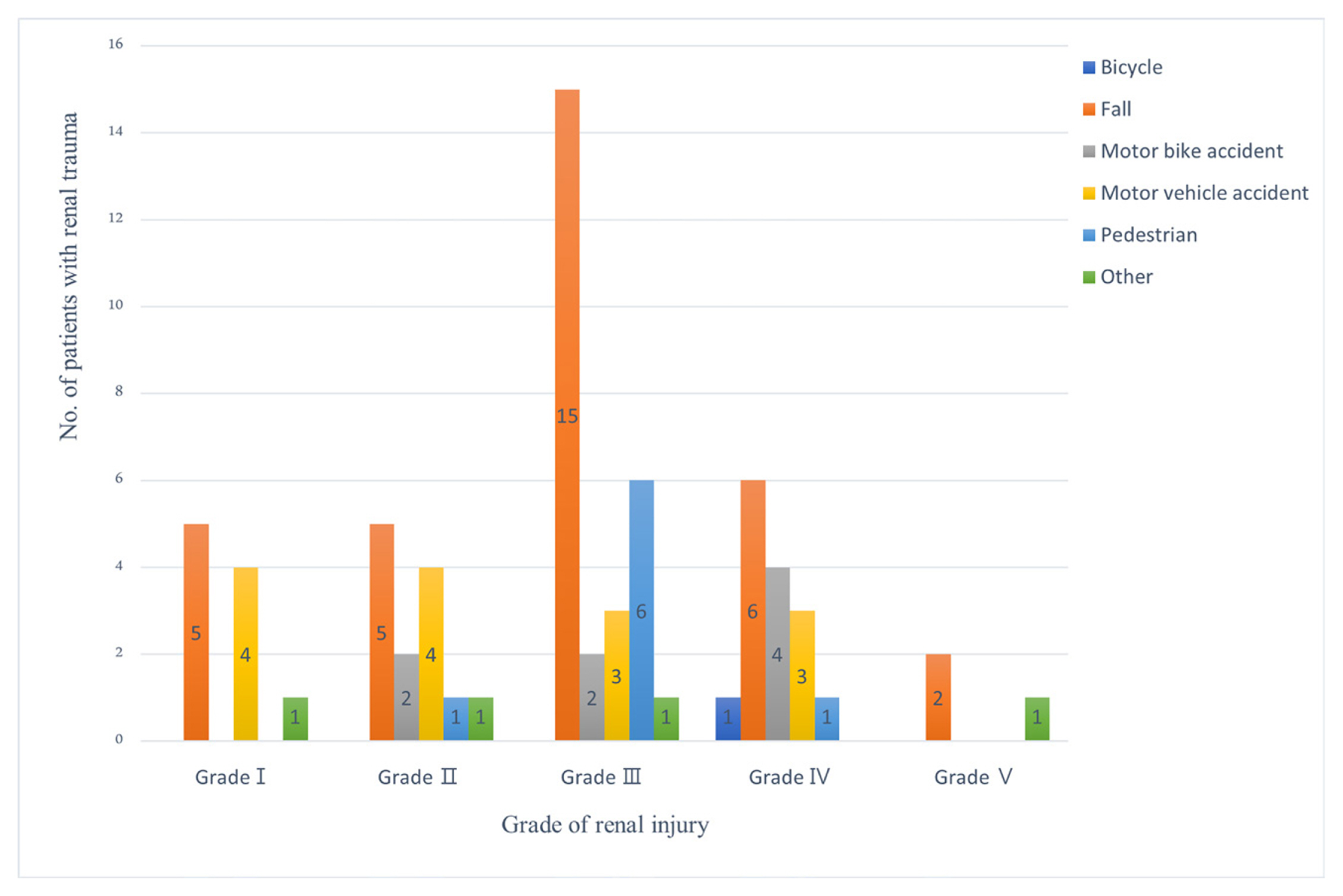
The median age of the patients was 52 years (interquartile range 33ŌĆō61 years), and 75.0% of the patients were male (Table 1). Fall injuries were the most common cause of blunt kidney trauma (48.5%) followed by motor vehicle accidents (20.6%). The grade of renal injury according to the AAST Kidney injury scale and mechanism of injury are illustrated in Figure 1. There were 98.5% (n = 67) of the patients who were treated nonoperatively including embolization (n = 8), and ureteral stenting (n = 1; Table 1). Nephrectomy was performed in one patient, and the overall treatment mortality rate was 2.9% (n = 2; Table 1). One patient died of aggravated cerebral edema after surgery for traumatic subdural hemorrhage, and one patient died of sepsis related to intraperitoneal organ surgery.
In this study, 16 patients (23.5%) had isolated renal trauma, and injuries in the chest region (n = 39, 57.4%) which were most associated with renal trauma (Table 2).
Forty-five patients (66.2%) were high-grade renal injury patients. The numbers of patients with high-grade injury, tachycardia, hypotension, presence of transfusion, associated injury with renal injury, LOS in the intensive care unit, and overall mortality were higher than the number of patients with low-grade renal injury, but these differences were not statistically significant (Table 3). There was no statistically significant difference in nonoperative treatment including embolization, between the patients with high-grade injury (n = 44, 97.8%) and the patients with low-grade injury (n = 23, 100%; p = 0.511; Table 3). Nonoperative treatment was performed in all patients with low-grade renal injury, and eight cases of embolization, one case of ureteral stenting, and one case of nephrectomy were performed in patients with high-grade renal injury (Figure 2).
Non-surgical treatment is recommended as the treatment of choice for hemodynamically stable or stable high-grade blunt renal injury [3]. In this study, 66.2% (n = 45) of blunt renal injury patients (n = 68) had high-grade injury. Nonoperative management including embolization and ureteral stenting was successful in 97.8% (n = 44) of the high-grade renal injury group.
During the initial resuscitation of trauma patients, intra-abdominal organ bleeding can be diagnosed rapidly using sonography to perform a focused assessment of the trauma [12ŌĆō14]; however, in the case of kidney injury, early diagnosis is difficult because of the anatomical location of the kidney. Advances in CT imaging and embolization have enabled a high success rate detecting the location and nonsurgical treatment of bleeding in cases of damage to solid abdominal organs such as the liver and spleen [15ŌĆō17]. The accumulation of skill in nonsurgical treatment of solid organs has made it possible to change the treatment paradigm from surgical (performing a nephrectomy) to conservative treatment of renal injury.
The kidney is only held in position by the renal pelvis and vascular pedicle, therefore, it is particularly vulnerable to decelerating injuries, such as falls, and motor vehicle collisions [3]. Studies have shown that falls and car accidents are the most common causes of renal injury [2,5,18,19]. In a retrospective study over 15 years, using data from the Japan Trauma Data Bank, patients with blunt renal trauma were identified (n = 3,550) and falls accounted for 34% of injuries, and car accidents accounted for 15.7% [18]. Another retrospective study over 8 years using the Taiwan National Trauma Bank (n = 10,096) reported that the most common mechanisms of renal injury were motor vehicle accidents (49.4%) and falls (27.4%) [19]. Motor vehicle accidents have been reported to be the most common cause of high-grade renal injury [2,5]. In cases of renal injury caused by high-energy mechanisms such as falls or traffic accidents, the incidence of high-grade renal injury is reported to be between 47.4% and 76% [1,2,18,20]. The mechanism of injury in the present study showed that 32 patients (48.5%) had experienced a fall, and 20.6% had been in a motor vehicle accident. Falls accounted for 51.1% and motor vehicle accidents for 13.3% cases of high-grade renal injury. The incidence rate of high-grade renal injury was 66.2%, which was similar to that reported by other institutions.
The high-energy impact that results in renal injury can also damage adjacent structures including the liver, spleen, and other abdominal organs, resulting in multiple injuries. Several studies have reported that patients with traumatic kidney injury often have concomitant injuries to other organs [1,4,20ŌĆō23]. In a Danish retrospective study, 58% (n = 107) of patients had injuries to other organs [20]. In an American study of 206 adult patients with Grade 4 or 5 blunt renal injury; concomitant injuries were observed in 94.2% of patients who underwent immediate surgery and 74.7% of those who received nonoperative management [21]. A study conducted in South Africa reported that associated organ injury occurred in 68.5% of cases, and the frequency of intra-abdominal organ injuries due to blunt trauma was highest in the liver (44.4%), followed by the spleen (31.5%) [4]. In a retrospective study of the Japan Trauma Bank, 85.7% of patients with blunt renal injury had multiple injuries, with associated intra-abdominal organ injury in the liver (27.3%) and spleen (18.5%) [18]. Our data showed that concomitant injuries occurred in 53 of the 68 patients (76.5%) and 35 of the 45 patients (77.8%) with high-grade blunt renal injury. Associated intra-abdominal organ injuries occurred in 16.2% in the liver, 14.7% in the adrenal glands, and 10.3% in the spleen.
Advances in radiological techniques and selective treatment with interventional radiology have reduced the need for surgical treatment, even for high-grade renal injury. A study by Khoschnau et al [2], reported that among 152 patients hospitalized for blunt renal injury, most (93%) patients were treated conservatively including those with high-grade renal injury. Salem et al [4] reported conservative treatment outcomes in 80.8% of patients with high-grade blunt renal injury, and Ōēź 78.8% of all patients in their five-year trauma management experience report. The authors suggested that, even with high-grade renal injury, nonsurgical treatment is safe and was associated with good outcomes [4]. The results of the AAST Genitourinary Trauma Study reported by Keihani et al [22] in 2018, showed that although penetrating injuries were often treated with nephrectomy, more than 90% of patients with blunt trauma can be treated conservatively. Nonoperative management is recommended for patients with hemodynamically stable or stabilized severe lesions without other reasons for surgical exploration [3]. However, in a survey of practice patterns for the treatment of high-grade renal trauma, of 253 practitioners, 95% of respondents agreed to preserve the kidney, but 50% of practitioners actually performed a nephrectomy for acute renal trauma management such as in case of severe renal bleeding within the first 4 hours of arrival or an exploratory laparotomy for other abdominal injuries with renal bleeding [23]. These results are consistent with those of a multicenter AAST study that showed that a nephrectomy was the most common intervention for bleeding in advanced trauma in 13% of cases, whereas angioembolization was performed in only 6% of patients [22]. Angioembolization of renal injuries is associated with a high success rate, even in patients with high-grade injuries [3,24]. In the present study, nonoperative management was performed in 98.5% of all patients, and was successful in 97.8% of patients with high-grade renal injuries.
This study has several limitations. Firstly, the data were retrospectively collated from medical records, and no randomization technique was applied. Secondly, this study included only a small number of patients who were admitted to a single institution. The small sample size may have reduced statistical power and thus the significance of the results obtained. Selecting a treatment method for blunt kidney injury can differ depending on the attending physician who makes the treatment decision, which results in variations in management. To resolve these limitations, a prospective, multicenter, large-scale study is required.
In conclusion, even with a high-grade renal injury, most patients with a traumatic renal injury can be managed with nonoperative treatment including angioembolization, and can have a good prognosis. The decision-making process for treatment options should be individualized for each patient, but nonoperative management should be considered whenever possible.
Notes
Author Contributions
Concept: KKH. Design: KKH. Supervision: KKH. Materials: KJS. Data Collection and/or Processing: KSH. Analysis and/or Interpretation: KSH. Literature Search: KJS. Writing Manuscript: KJS and KKH. Critical Review: KKH.
Figure┬Ā1
Distribution of renal injuries by mechanism and American Association for the Surgery of Trauma scale.
Table┬Ā1
Demographics of patients with blunt renal trauma (age > 18).
Table┬Ā2
Injures of organs related to renal injury (age >18).
Table┬Ā3
Differences between low-grade and high-grade blunt renal injury.
References
1. Syarif , Palinrungi AM, Kholis K, Palinrungi MA, Syahrir S, Sunggiardi R, et al. Renal trauma: a 5-year retrospective review in single institution. Afr J Urol 2020;26:61.


2. Khoschnau S, Jabbour G, Al-Hassani A, El-Menyar A, Abdelrahman H, Afifi I, et al. Traumatic kidney injury: an observational descriptive study. Urol Int 2020;104(1ŌĆō2):148ŌĆō55.



3. Coccolini F, Moore EE, Kluger Y, Biffl W, Leppaniemi A, Matsumura Y, et al. Kidney and uro-trauma: WSES-AAST guidelines. World J Emerg Surg 2019;14:54.




4. Salem MS, Urry RJ, Kong VY, Clarke DL, Bruce J, Laing GL. Traumatic renal injury: five-year experience at a major trauma centre in South Africa. Injury 2020;51(1):39ŌĆō44.


5. Sarang B, Raykar N, Gadgil A, Mishra G, Warnberg MG, Rattan A, et al. Outcomes of renal trauma in Indian urban tertiary healthcare centres: A multicentre cohort study. World J Surg 2021;45(12):3567ŌĆō74.




6. Erlich T, Kitrey ND. Renal trauma: the current best practice. Ther Adv Urol 2018;10(10):295ŌĆō303.




7. Smith EM, Elder JS, Spirnak JP. Major blunt renal trauma in the pediatric population: is a nonoperative approach indicated? J Urol 1993;149(3):546ŌĆō8.


8. Buckley JC, McAninch JW. Selective management of isolated and nonisolated grade IV renal injuries. J Urol 2006;176(6 Pt 1):2498ŌĆō502. discussion 2502.


9. Serafetinides E, Kitrey ND, Djakovic N, Kuehhas FE, Lumen N, Sharma DM, et al. Review of the current management of upper urinary tract injuries by the EAU Trauma Fuidelines Panel. Eur Urol 2015;67(5):930ŌĆō6.

10. Bjurlin MA, Fantus RJ, Fantus RJ, Villines D. Comparison of nonoperative and surgical management of renal trauma: can we predict when nonoperative management fails? J Trauma Acute Care Surg 2017;82(2):356ŌĆō61.

11. Kozar RA, Crandall M, Shanmuganathan K, Zarzaur BL, Coburn M, Cribari C, et al. Organ injury scaling 2018 update: spleen, liver, and kidney. J Trauma Acute Care Surg 2018;85(6):1119ŌĆō22.


12. Jansen JO, Yule SR, Loudon MA. Investigation of blunt abdominal trauma. BMJ 2008;336(7650):938ŌĆō42.



13. Healey M, Simons RK, Winchell RJ, Gosink BB, Casola G, Steele JT, et al. A prospective evaluation of abdominal ultrasound in trauma: is it useful? J Trauma 1996;40(6):875ŌĆō83. discussion 883ŌĆō5.

14. Rozycki GS, Ballard RB, Feliciano DV, Schmidt JA, Pennington SD. Surgeon-performed ultrasound for the assessment of truncal injuries: lessons learned from 1540 patients. Ann Surg 1998;228(4):557ŌĆō67.


15. Wallis A, Kelly MD, Jones L. Angiography and embolization for solid abdominal organ injury in adults- a current perspective. World J Emerg Surg 2010;5:18.



16. Kiankhooy A, Sartorelli KH, Vane DW, Bhave AD. Angiographic embolization is safe and effective therapy for blunt abdominal solid organ injury in children. J Trauma 2010;68(3):526ŌĆō31.


17. Coccolini F, Catena F, Moore EE, Ivatury R, Biffl W, Peitzman A, et al. WSES classification and guidelines for liver trauma. World J Emerg Surg 2016;11:50.




18. Nakao S, Katayama Y, Hirayama A, Hirose T, Ishida K, Umemura Y, et al. Trends and outcomes of blunt renal trauma management: a nationwide cohort study in Japan. World J Emerg Surg 2020;15(1):50.




19. Hsu CP, Cheng CT, Huang JF, Fu CY, Bajani F, Bokhari M, et al. The effect of transarterial embolization versus nephrectomy on acute kidney injury in blunt renal trauma patients. World J Urol 2022;40(7):1859ŌĆō65.



20. Maibom SL, Holm ML, Rasmussen NK, Germer U, Joensen UN. Renal trauma: a 6-year retrospective review from a level 1 trauma center in Denmark. Scand J Urol 2019;53(6):398ŌĆō402.


21. Van der Wilden GM, Velmahos GC, Joseph DK, Jacobs L, Debusk MG, Adams CA, et al. Successful nonoperative management of the most severe blunt renal injuries: a multicenter study of the research consortium of New England Centers for Trauma. JAMA Surg 2013;148(10):924ŌĆō31.


22. Keihani S, Xu Y, Presson AP, Hotaling JM, Nirula R, Piotrowski J, Dodgion CM, et al. Contemporary management of high-grade renal trauma: results from the American Association for the Surgery of Trauma Genitourinary Trauma study. J Trauma Acute Care Surg 2018;84(3):418ŌĆō25.


-
METRICS

-
- 0 Crossref
- 1,155 View
- 50 Download
-
Related articles in
J Acute Care Surg -
Management of Traumatic Duodenal Injuries: A Report from a Single-Center2022 March;12(1)