|
 |
- Search
| J Acute Care Surg > Volume 13(1); 2023 > Article |
|
Abstract
Few studies have reported injuries caused by a blank cartridge shot (BCS) into the head and neck. We experienced a case of minor injury resulting from BCS (despite the close proximity). The patient was a 20-year-old male soldier who attempted suicide by firing a BCS from a K2 rifle into his mouth. He suffered from skin and soft tissue defect in the submandibular area with burns and minimal bleeding. A computed tomography scan showed subcutaneous emphysema which was suspected to be related to the projectile gas released during the firing of the BCS, and a tiny fragment without hematoma or structure injuries. We closely observed the clinical features including the occurrence of infection and functional abnormalities. The subcutaneous emphysema faded away along with the soft tissue defect. After wound management was completed on the 13th hospital day, the patient was transferred to the Department of Psychiatry without any problems.
In South Korea, clinicians rarely encounter patients with gunshot wounds because the general civilian population are prohibited from having guns (except for people in law enforcement). However, military clinicians occasionally encounter military personnel with gunshot wounds resulting from accidental events, military crimes, or suicide attempts. Although there are cases of blank cartridge shot (BCS) in patients with gunshot injuries, few studies about BCS have been reported.
BCS is generally accepted as harmless, however, there is a ballistics study which reports that BCS injury from a distance of 50 cm could be fatal [1]. In addition, some studies have reported serious cases caused by BCS including fatalities [2,3]. However, estimations of BCS injuries should be avoided because it could lead to an overestimation of BCS injuries and unnecessary studies.
Serious injuries caused by BCS are rarely reported. Minor injuries from BCS are extremely rare. In this study, a case of minor injury is reported which resulted from a BCS, despite the close proximity from which the gun was fired. This case report was approved by the institutional review board (IRB) of Armed Forces Trauma Center, Armed Forces Capital Hospital (IRB no.: AFCH 2022-12-002). The study adhered to the tenets of the Declaration of Helsinki.
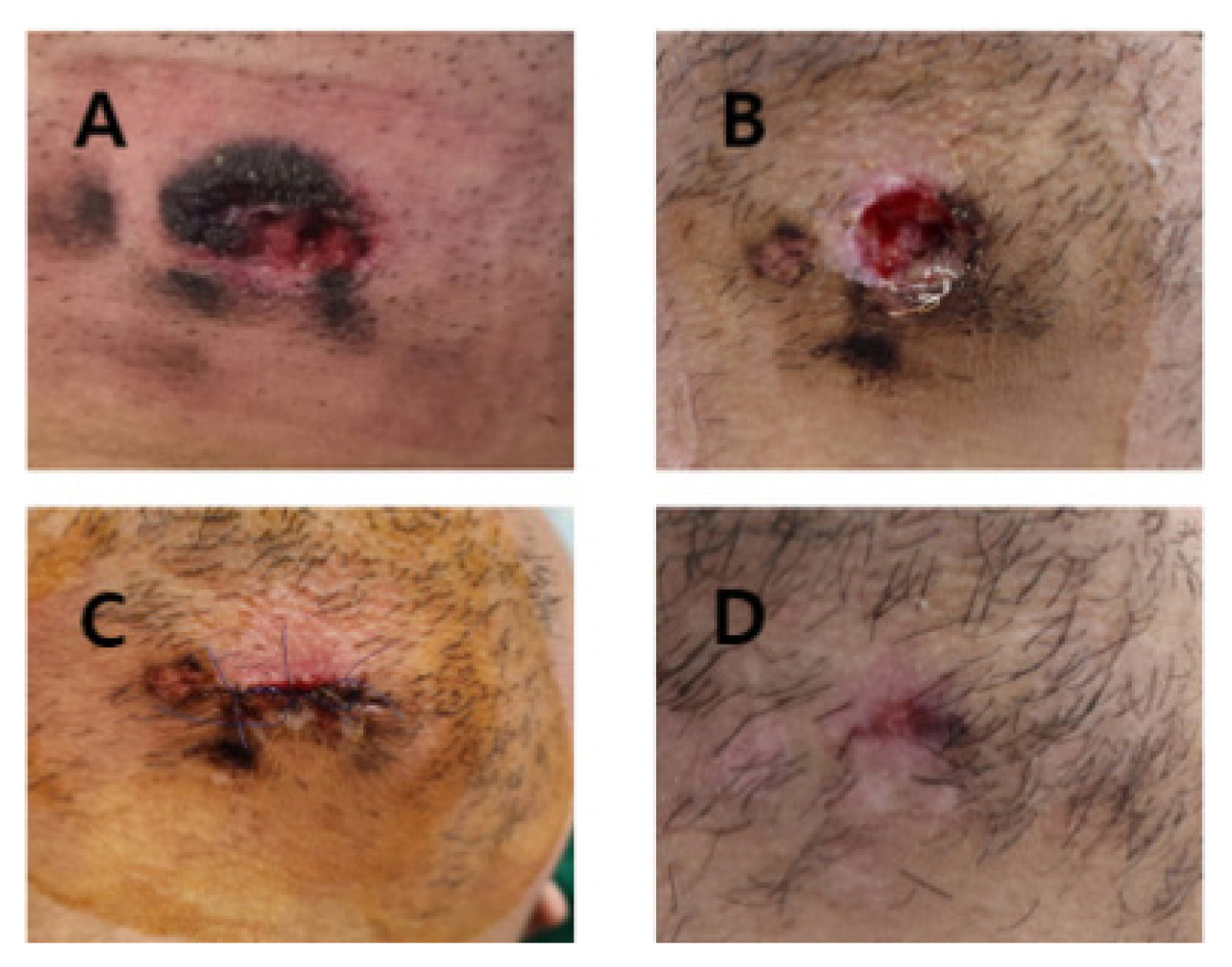
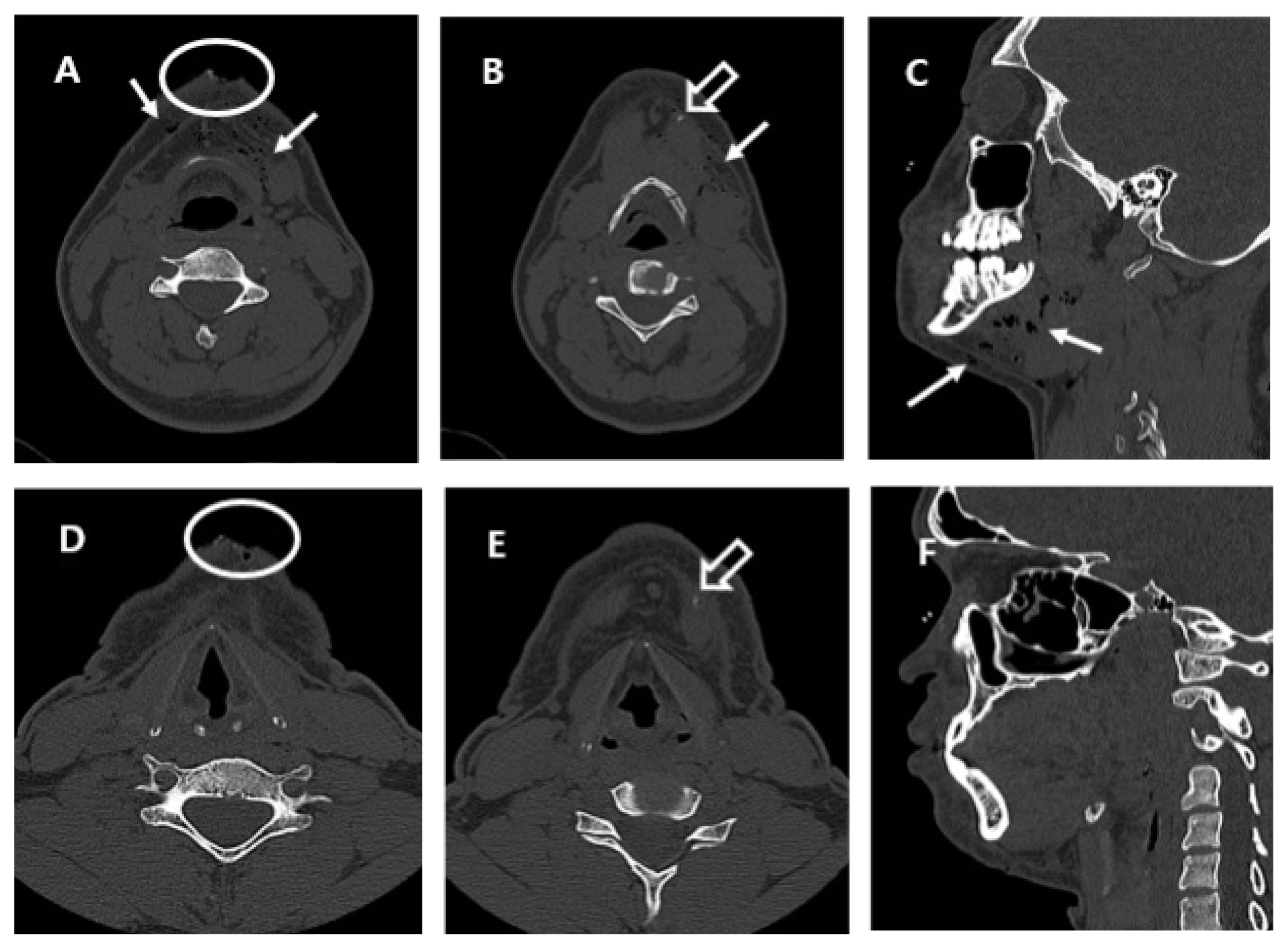
A 20-year-old male soldier with submandibular wounds (Figure 1A) was admitted to the emergency room of Armed Forces Trauma Center, Armed Forces Capital Hospital in South Korea. The wound was caused by a BCS from a K2 rifle into the submandibular area in a suicide attempt. It was round and had a diameter of 2 cm, with skin burn on the edge of the wound and minimal bleeding. At the time of admission his vital signs were measured, his blood pressure was 104/71 mmHg, his breathing was 15 breaths per minute, his pulse was 59 beats per minute, and his temperature was 36.6┬░C. His Glasgow coma scale score was 15. There was no sign of bleeding (such as swelling or bruises), respiratory distress, or any problems speaking. As the patient did not require emergency exploration, a facial computed tomography (CT) scan was performed. On the CT scan, a subcutaneous emphysema in the facial soft tissue was observed without hematoma or any structural injury, and a tiny fragment was also observed (Figures 2A, 2B and 2C).
We performed simple dressing and administered oral antibiotics (amoxicillin/clavulanate) because of the possibility of infection from the gunpowder and the wound. On the follow-up CT on the 6th day, the subcutaneous emphysema had faded away with the soft tissue defect replaced with regenerated tissue (Figures 2D, 2E and 2F). We did not remove the tiny fragment in the submandibular soft tissue (Figure 2E) because inflammation was not observed. In addition, its removal could lead to unnecessary complications such as bleeding and infection. The skin defect was then repaired because the wound was clear without signs of infection or inflammation (Figures 1B and 1C). The stitches were removed 4 days later.
On 13th hospital day, the patient was transferred to Department of Psychiatry without any problems after wound management had been completed (Figure 1D).
Penetrating injury to the head and neck often have life-threatening features such as airway injury and rupture of major vessels [4ŌĆō7]. Gunshot commonly causes serious injury, and although several cases of injuries caused by BCS have been reported, description about features and management of the injuries are insufficient [2,3,8]. The blank cartridge is designated to have the fire sound and gas flare from the gun without the bullet. Its gunpowder and projectile gas could cause injury to human body [2]. Injuries from BCS vary in severity ranging from minor to fatal. Therefore, clinicians encountering patients with injuries from a BCS should decide the treatment plan on a case-by-case basis.
The severity of BCS injury could be related injury site. In a previous report, a patient who sustained injury from a BCS into his oral cavity underwent tracheal intubation immediately to keep his airway open because his mouth had filled with blood, which was followed by a tracheostomy to examine and operate in the oral cavity [8]. The patient suffered from severe soft palate injury. He then underwent emergency operation for bleeding control. He had to keep the tracheostomy tube for a long period during recovery [8]. In another report, a mortality case, where the BCS was fired at close range into the temporal region where it led to a brain hemorrhage and edema [9]. Where there is a BCS into the head (including face) and neck the possible injuries that should be considered include injury to the airway, major vessels, and brain. Therefore, clinicians who encounter these patients should examine airway, breathing, circulation, and disability (neurologic sign) as a priority [6].
In many cases of penetrating injury into the face and neck, exploration is performed for bleeding control, and for detecting and managing structural injuries [4ŌĆō7]. However, performing exploration of the face and neck should be carefully considered because invasive exploration of these areas can lead to severe complications [10]. Surgical exploration should be performed with a definite purpose such as bleeding control, and the repairing of major structures. If patients who underwent penetrating injury of the face or neck presented with ongoing bleeding, respiratory distress, and any life-threatening situation, exploration should be performed as soon as possible without imaging or laboratory studies [6,7]. However, for patients who are stable and alert, without bleeding, or any critical signs, additional studies and an in-depth physical examination should be performed [11].
Subcutaneous emphysema in the face and neck could indicate injury of the airway, oropharynx, and esophagus [12]. If injuries are caused by blunt trauma or a penetrating stab wound, the clinician should consider emergency exploration. However, projectile gas from a BCS could lead to subcutaneous emphysema without causing other structural injuries. If a patientŌĆÖs vital signs are stable, additional studies should be performed, especially CT [13,14]. A patient without critical signs or abnormal image findings should be just observed closely.
In addition, since the gun powder and tiny fragment could be sources of infection, prophylactic antibiotics, and close observation are needed. Indications for removing a residual foreign body are as follows: (1) where the residual foreign body is located adjacent to the airway of the gastrointestinal tract, it needs to be removed. It will enter the lumen of the airway or gastrointestinal tract causing secondary bleeding or infection and psychological stress to the patient if not removed; (2) if the residual foreign body is located inside a vital organ such as an eyeball, the central nervous system, or the heart, it can be removed; (3) if the residual foreign body size is larger than 15 mm and located in the thorax or abdominal cavity, removal should be considered. In addition, the clinician should carefully observe for signs of lead poisoning during a 4ŌĆō6-week period, even though cases of lead poisoning from residual bullets have rarely been reported [15].
In conclusion, injuries from a BCS fired at close proximity could show various features, and generally may cause more serious injuries, however, injury is not inevitable. The clinician should carefully decide the course of action before performing an exploration.
Notes
Author Contributions
Conceptualization and formal analysis: KL. Writing original draft: KL. Writing-review and editing: HJL, DL and KL.
Ethical Statement
This study was approved by the IRB of the Armed Forces Capital Hospital (IRB no.: AFCH 2022-12-002) and adhered to the tenets of the Declaration of Helsinki. The requirement for informed consent was waived by IRB of Armed Forces Hospital because of the retrospective nature of this study. All personal identification of the patient was removed.
Figure┬Ā1
Submandibular wound caused by a blank cartridge shot: (A) in the emergency room; (B) on the 6th HD, the wound was clear and regeneration of tissue was partial; (C) state of wound repair on the 6th HD; (D) nearly complete healing on the 13th day.
HD = hospital day.
Figure┬Ā2
Images of facial computed tomography scan: (A, B, and C) in the emergency room, subcutaneous emphysema in the mandibular area, soft tissue defect at the submandibular site, and a tiny fragment were observed; (D, E and F) on the 6th HD, subcutaneous emphysema faded out and the soft tissue defect was partially covered with regenerated tissue. A tiny fragment was observed.
arrow-empty = a tiny fragment; arrow-white = subcutaneous emphysema; circle = soft tissue defect; HD = hospital day.
References
1. Rabl W, Riepert T, Steinlechner M. Metal pins fired from unmodified blank cartridge guns and very small calibre weapons--technical and wound ballistic aspects. Int J Legal Med 1998;111(4):219ŌĆō23.



2. G├╝l┼¤en I, Ak H, Sosuncu E, Bulut MD. Are blank cartridge guns really harmless? Ulus Travma Acil Cerrahi Derg 2014;20(3):214ŌĆō6.


3. Zdravkovic M, Milic M, Stojanovic M, Kostov M. Three cases of death caused by shots from blank cartridge. Am J Forensic Med Pathol 2009;30(4):403ŌĆō6.


4. Khan AM, Fleming JC, Jeannon JP. Penetrating neck injuries. Br J Hosp Med (Lond) 2018;79(2):72ŌĆō78.


5. Brockhoff HC 2nd, Morris C, Tiwana P, Bebeau N, Phillips C. Vessel injuries of the head and neck presenting in mandibular fractures. Oral Surg Oral Med Oral Pathol Oral Radiol 2014;118(3):267ŌĆō70.


6. Verdonck P, de Schoutheete JC, Monsieurs KG, Van Laer C, Vander Poorten V, Vanderveken O. Penetrating and blunt trauma to the neck: clinical presentation, assessment and emergency management. B-ENT 2016;Suppl 26(2):69ŌĆō85.

7. Shiroff AM, Gale SC, Martin ND, Marchalik D, Petrov D, Ahmed HM, et al. Penetrating neck trauma: a review of management strategies and discussion of the 'No Zone' approach. Am Surg 2013;79(1):23ŌĆō9.



8. Lee H, Hwang K, Lee Y, Jeong SY. Survival of a Blank Cartridge Gunshot Injury to the Soft Palate in a Soldier. J Craniofac Surg 2022;33(6):e573ŌĆō6.


9. Buyuk Y, Cagdir S, Avsar A, Duman GU, Melez DO, Sahin F. Fatal cranial shot by blank cartridge gun: two suicide cases. J Forensic Leg Med 2009;16(6):354ŌĆō6.


10. Miller RH, Duplechain JK. Penetrating wounds of the neck. Otolaryngol Clin North Am 1991;24(1):15ŌĆō29.


11. Kendall JL, Anglin D, Demetriades D. Penetrating neck trauma. Emerg Med Clin North Am 1998;16(1):85ŌĆō105.


12. Hajiioannou J, Sioka E, Koukoura O, Bizakis J. Subcutaneous emphysema to the head and neck: an unlikely traumatic origin. BMJ Case Rep 2018;2018:bcr2018224380..



-
METRICS

-
- 1 Crossref
- 1,056 View
- 40 Download
-
Related articles in
J Acute Care Surg