Introduction
Splenic abscess is an uncommon entity encountered during surgical practice. It is the immunocompromised patient who is prone to development of splenic abscess and its associated complications [1]. The majority of patients present with nonspecific symptoms in the form of malaise, weight loss, fever, abdominal pain, nausea, and vomiting. The classical triad of fever, tenderness in left upper abdomen, and leukocytosis is only present in one third of the patients [2]. Rupture of a splenic abscess can lead to complications like peritonitis (localized or generalized), left pleural effusion, pneumonia, and subphrenic abscess [3]. Here we report the case of an immunocompetent patient who presented with splenic abscess rupture which led to pneumoperitoneum and hence a misdiagnosis of hollow viscera perforation.
Case Report
A 32-year old male presented as a surgical emergency with complaints of pain abdomen for the past 3 days. It was sudden in onset and started in the left side of his abdomen and gradually progressed to the whole abdomen. The pain was severe in intensity and showed no improvement with medication. Multiple episodes of undocumented high-grade fever were also present. The pain and fever were associated with non-passage of stools and flatus. There was no history of comorbidities like diabetes mellitus, hypertension, thyroid disorder, or tuberculosis. The patient used to smoke 1bundle of bidi per day for the past 15 years.
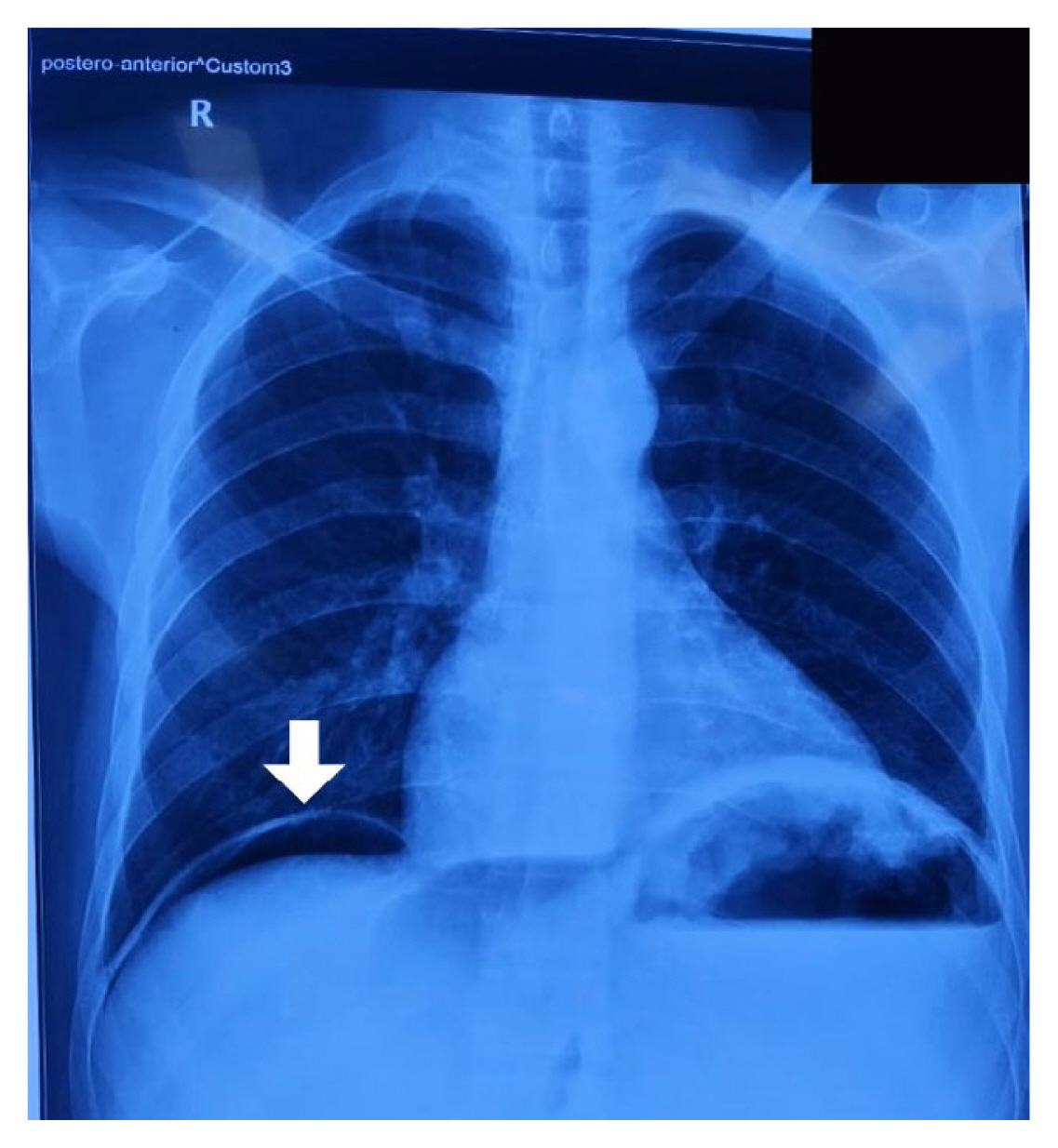
On initial assessment, the patient was average built. He was febrile to touch and had a temperature of 38.3 ºC (101 ºF). His pulse rate was 130 beats/minute and he had a blood pressure of 90/60 mmHg. Abdominal examination revealed a tense, distended abdomen with generalized tenderness, guarding and rigidity, and features consistent with peritonitis. On auscultation, bowel sounds were absent. Complete blood counts showed anemia (6.1 gm/dL) with mild leukocytosis (15,900/mm3). The serum renal function test showed elevated blood urea nitrogen and creatinine which suggested prerenal acute kidney injury. An upright chest radiograph scan was performed which showed the presence of free air under the right dome of the diaphragm (Figure 1). On clinical radiological correlation, the provisional diagnosis of perforation peritonitis was made. The patient was started on intravenous fluids and broad-spectrum antibiotics. A nasogastric tube and per urethral Foley’s catheter were inserted.
Consistent with the clinical features of peritonitis, radiological features of pneumoperitoneum, and a background of chronic smoking, a provisional diagnosis of upper gastrointestinal tract perforation was made. Since emergency laparotomy is the standard management approach for peritonitis, the patient was taken for operative intervention without delay. Additional radiological investigations (computerized tomography of the abdomen) were not performed because the results would not have changed the management plan.
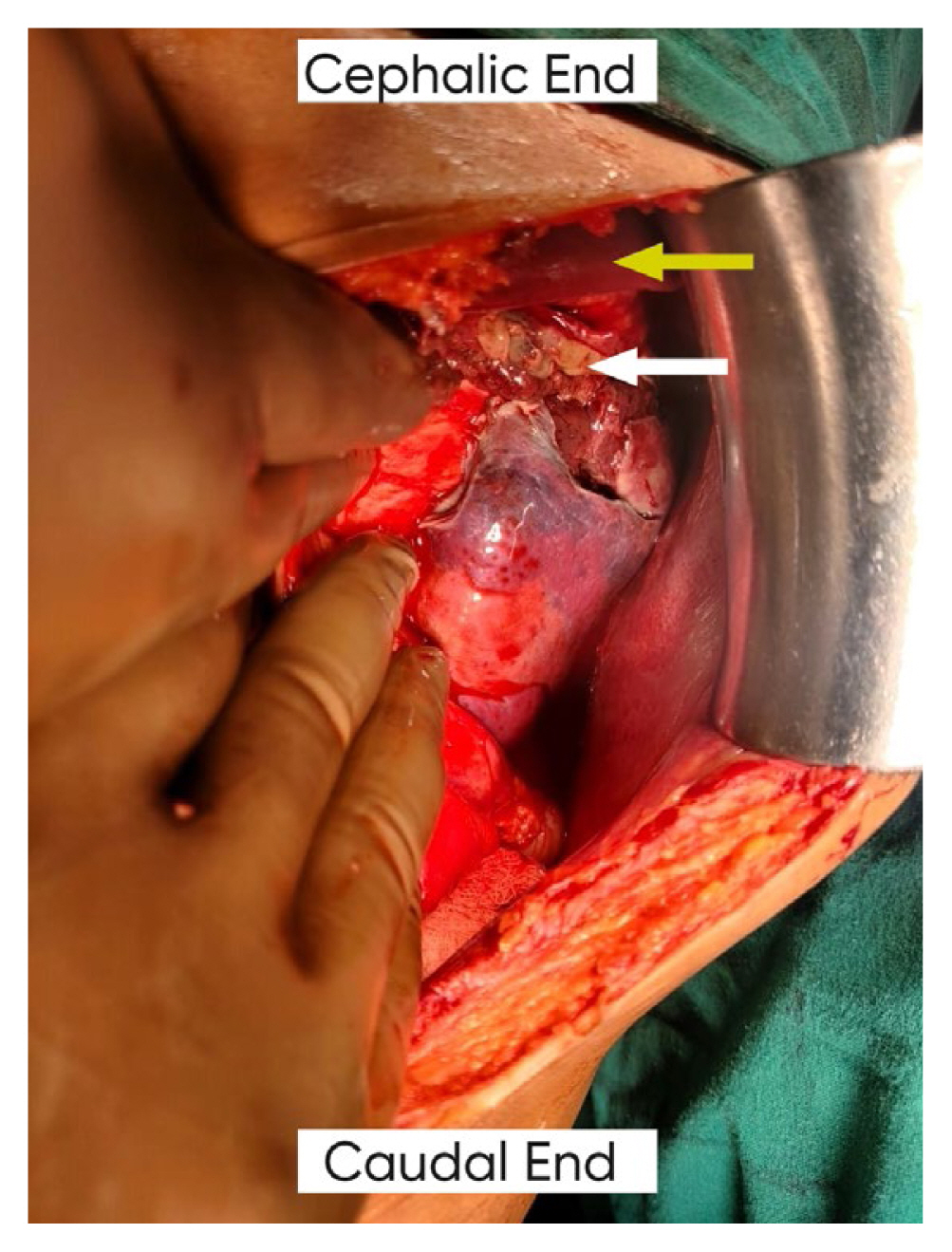
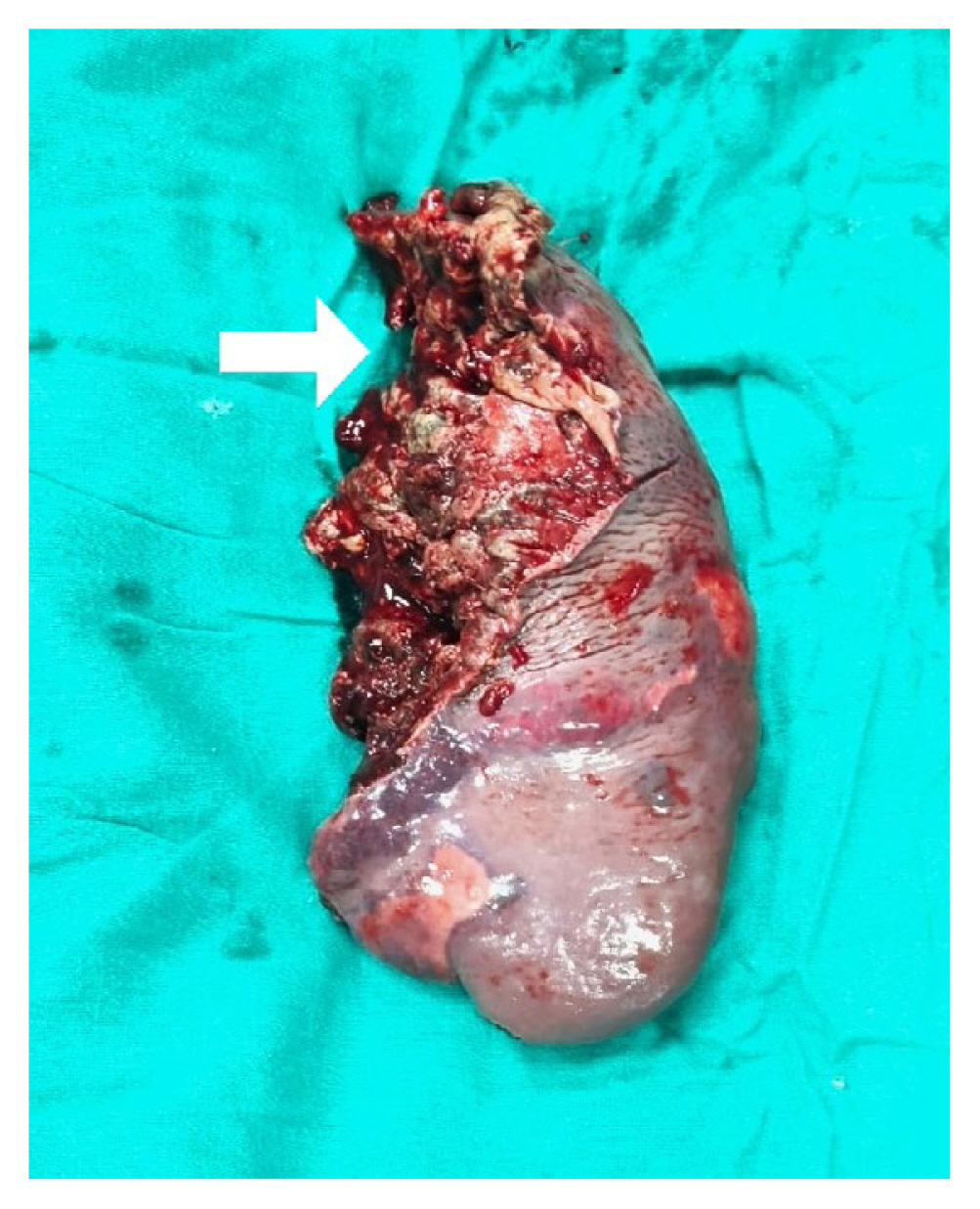
The patient was explored as an emergency via a midline laparotomy incision. On opening the peritoneum, a gush of air was released and pus came out. Approximately, 1L of purulent fluid was drained. Thorough abdominal lavage was performed. The bowel was examined and no perforation was identified. We found an abscess located at the upper pole of the spleen, which had ruptured into the peritoneal cavity (Figure 2). Since the spleen was necrotic, a splenectomy was performed, and a left paracolic drain was placed.
No postoperative complications occurred. The drain was removed on 2nd postoperative day, and the patient was discharged on antibacterial drug therapy. Post splenectomy vaccines against pneumococcus, meningococcus, and haemophilus influenza were administered.
Histopathological examination of the specimen revealed splenomegaly with necrotic tissue and a rupture measuring 10 × 8.5 × 3 cm (Figure 3). On microscopy, inflammatory infiltrate and coagulative necrosis were observed. Ziehl Neelson stain for acid fast bacilli was negative and, no fungal elements were detected following periodic acid-Schiff stain.
In the post operative period various investigations were carried out to determine the cause of the splenic abscess. Bone marrow examination and the leukocyte alkaline phosphatase test for suspicion of haemoglobinopathies showed normal results. Infective endocarditis was excluded as an etiology of the abscess by performing an echocardiogram, which was reported as normal. The pus culture showed growth of Escherichia coli whereas the blood culture was sterile after 48 hours of incubation. There was no history suggestive of abdominal trauma which would indicate an infected splenic hematoma as a diagnosis.
Discussion
Splenic abscess is a rare clinical entity with an incidence of 0.1% to 0.7% on autopsy studies. Mortality rates as high as 47% have been reported, which can rise to 100% in the absence of appropriate and timely management [4]. The patients predisposed to splenic abscesses are those suffering from immunocompromised conditions (diabetes mellitus, HIV), neoplasia, intravenous drug abuse, abdominal trauma, and infective endocarditis to name a few [5]. It is an uncommon entity in an immunocompetent patient like the case in this report. A few studies mention that splenic abscesses usually present in patients with fever (89%), left upper quadrant pain (84%), and leukocytosis over 11,000/mm3 (67%)[6]. The classical triad where the 3 symptoms mentioned above are present simultaneously is observed in as few as one-third of patients [2]. These symptoms are nonspecific, and may be present in other acute abdomen etiologies, thus adding to the diagnostic dilemma. Our patient did present with the classical triad but we did not consider splenic abscessin our provisional diagnosis owing to the rare nature of this condition. Rather we considered his symptoms as a case of perforation peritonitis and performed an emergency exploratory laparotomy.
The patients with splenic abscesses may present initially with pyrexia of unknown origin. Rupture of the abscess may lead to complications like left pleural effusion, pneumonia, left subphrenic abscess, and localized left abdominal peritonitis [3]. Our patient presented with generalized peritonitis.
A recent retrospective study by Chang et al [2] on 67 patients with splenic abscesses showed 71.6% of patients had a solitary splenic abscess, while the remaining patients had multiple abscesses. Microbiological cultures were positive in 86.6% patients, with blood cultures 71.8% positive and abscess cultures 93.5% positive. Gram negative bacillus infection predominated (55.2%), followed by gram positive coccus infection (31%). In the current case the abscess was solitary, and the pus culture revealed the presence of Escherichia coli, while the blood culture was sterile.
Computerized tomography of the abdomen is the preferred imaging modality when there is a clinical suspicion of splenic abscess [7]. However, in some cases, the diagnosis is made intraoperatively, as in our case. Treatment options for splenic abscess vary, ranging from conservative management (broad spectrum antibiotics, percutaneous drainage/aspiration) to operative intervention (splenectomy) [8]. Decisions should be made on a case by case basis because formal treatment guidelines are poorly defined. Conservative management may be an option if preoperative diagnosis of splenic abscess is made. However, if the diagnosis is made intraoperatively a splenectomy may be necessary. Failure of conservative management also warrants a splenectomy.
Splenic abscess is a rare entity, especially among immunocompetent people. Splenic abscess presenting with pneumoperitoneum is even more rare. Nonspecific clinical findings lead to delayed diagnosis, resulting in delayed management and hence increased mortality. Thus, timely diagnosis and intervention (conservative/operative) is the key to successful management.