Introduction
Chronic cor pulmonale is a condition characterized by right ventricular hypertrophy secondary to pulmonary disease, which accompanies severe pulmonary hypertension (PH) [1]. The method of anesthesia must be carefully considered for patients with chronic cor pulmonale and severe PH, as these patients have an increased risk of postoperative mortality and morbidity. Previous studies have recommended neuraxial block techniques, such as epidural anesthesia, for these patients [2]. Furthermore, analgesia provided by the epidural route is commonly recommended for patients with severe PH in order to inhibit surgical pain-induced stress and sympathetic tone [3]. Although the use of epidural opioid analgesia in combination with local anesthetics via the epidural route presents multiple advantages, opioid administration may induce potentially fatal respiratory depression. In particular, the toxicity and side effects of epidural opioids may cause more serious problems in older patients or patients with chronic pulmonary disease [4].
Here, we report the case involving a patient with a tuberculosis-destroyed lung who was diagnosed with chronic cor pulmonale accompanied by severe PH. Specifically, we report that hypercarbia developed during postoperative pain control at the surgical intensive care unit (ICU) following administration of the spinal-epidural anesthesia during non-cardiac surgery.
Case Report
A 43-year-old woman (height, 160 cm; weight, 42.5 kg) presented with a 12.5-cm mass in the left upper medial thigh and lower limb edema. She was diagnosed with synovial sarcoma and wide excision of the tumor was planned. She had respiratory restrictions due to a tuberculosis-destroyed lung and bronchiectasis that developed after she had contracted tuberculosis 20 years ago. She was receiving home oxygen therapy (1.5Ōł╝3 L/min) via a nasal cannula and has been maintaining 80% oxygen saturation.
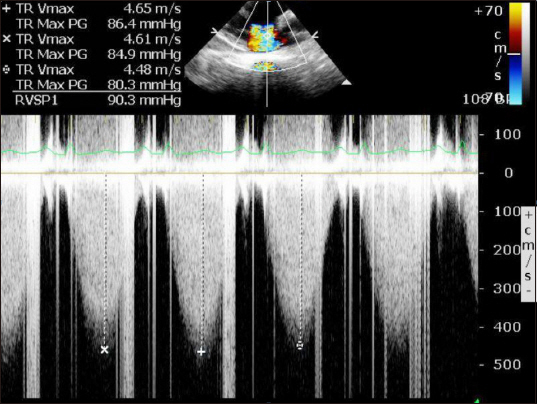
Chest computed tomography (CT) showed the tuberculosis- destroyed right lung and associated tuberculosis sequelae in the left lung. CT angiography showed enlargement of the right heart and pulmonary artery, meeting the criteria for cor pulmonale. Cardiac echographic findings suggested severe tricuspid regurgitation, severe PH (right ventricular systolic pressure=90.3 mmHg) (Fig. 1), a dilated right ventricle (RV) and right atrium, normal left ventricular contractility with an ejection fraction of 63%, RV hypokinesia, and moderate pericardial effusion. Brain-type natriuretic peptide was 2,342 pg/ml, and pulmonary function tests were not performed.
Preoperative vital signs at the ICU were as follows: blood pressure (BP), 95Ōł╝106/66Ōł╝76 mmHg; heart rate (HR), 89Ōł╝107 beats/min; and respiratory rate (RR), 18Ōł╝20/min. Oxygen saturation fluctuated heavily from 55Ōł╝88% depending on the patientŌĆÖs respiration and movement while receiving 3 L/min of oxygen via the nasal cannula. Arterial blood gas analysis (ABGA) findings on the morning of the operation were as follows: pH, 7.39; partial pressure of carbon dioxide (PaCO2), 51.6 mmHg; partial pressure of oxygen (PaO2), 72.2 mmHg; bicarbonate (HCO3-), 28.5 mmol/L. The patient did not complain of dyspnea and was fully conscious.
The patient was transferred to the operating room while receiving 3 L/min oxygen via a nasal cannula without premedication. As Electrocardiogram, pulse oxygen saturation, and non- invasive BP monitoring commenced, a 20-gauge needle was inserted into the right radial artery, and a 7-Fr double-lumen catheter was inserted into the right internal jugular vein. Combined spine-epidural anesthesia was performed with the patient in the left recumbent position at the third to fourth lumbar space using a midline approach. After administering 12.5 mg of heavy bupivacaine intrathecally, an epidural catheter was inserted. The patient was changed to the supine position to check the height of spinal anesthesia; sensory blockade reached the tenth thoracic segment after five minutes and the eighth thoracic segment after ten minutes, after which the patient was prepared for surgery. 100% Oxygen was supplied with a reservoir mask at 4 L/min. Respiratory patterns and expiratory CO2 concentration were monitored with an anesthetic machine and the concentration was well maintained without breathing difficulty. BP dropped to 78/42 mmHg 25 minutes after intrathecal injection of bupivacaine, and subsequently 30 ┬Ąg of phenylephrine was intravenously infused. At 35 minutes, 30 ┬Ąg of intravenous (IV) phenylephrine was additionally used, during which 2 mg of IV milrinone was infused over 10 minutes, after which it was continuously infused at 0.375 ┬Ąg┬Ękg-1┬Ęmin-1. Intraoperative ABGA showed pH 7.34, PaCO2 59.4 mmHg, PaO2 217 mmHg, and HCO3- 28.8 mmol/L. In response to a potential drop of BP following the administration of milrinone, an optimal dose of norepinephrine was intravenously infused at 0.02Ōł╝0.07 ┬Ąg┬Ękg-1┬Ęmin-1. BP was subsequently maintained at 85Ōł╝100/45Ōł╝60 mmHg. The operation commenced approximately 40 minutes after the intrathecal injection of bupivacaine. At 80 minutes following the intrathecal injection, 5 ml of 2% lidocaine was injected via the epidural catheter to confirm the intrathecal position of the catheter, and 10 ml was additionally infused at 90 minutes. At 100 minutes, epidural patient-controlled analgesia (PCA) (0.1875% ropivacaine, fentanyl 1.25 ┬Ąg/ml) was connected to begin continuous infusion at 2 ml/h with a bolus dose of 2 ml and a lockout time of 15 minutes. BP remained stable and so norepinephrine was stopped, followed by cessation of milrinone administration at 130 minutes. The surgery concluded without adverse events, and the patient was transferred to the ICU. The total duration of anesthesia and operative time were 2 hours and 55 minutes and 1 hour and 40 minutes, respectively. Intraoperative fluid levels included administration of 450 ml of crystalloid, urinary output was 115 ml, and less than 10 ml of estimated blood was lost.
ABGA at the ICU showed pH 7.3, PaCO2 66.4 mmHg, PaO2 50.1 mmHg, and HCO3- 27.9 mmol/L. The patient was conscious with no dyspnea, and her vital signs were BP 92/53 mmHg, HR 123 beats/min, RR 16 beats/min, and pulse oxygen saturation 67%. Oxygen was supplied with a nasal cannula at 3 L/min. The level of anesthesia was at T12, and pain score (numeric rating scale, NRS) was 0.
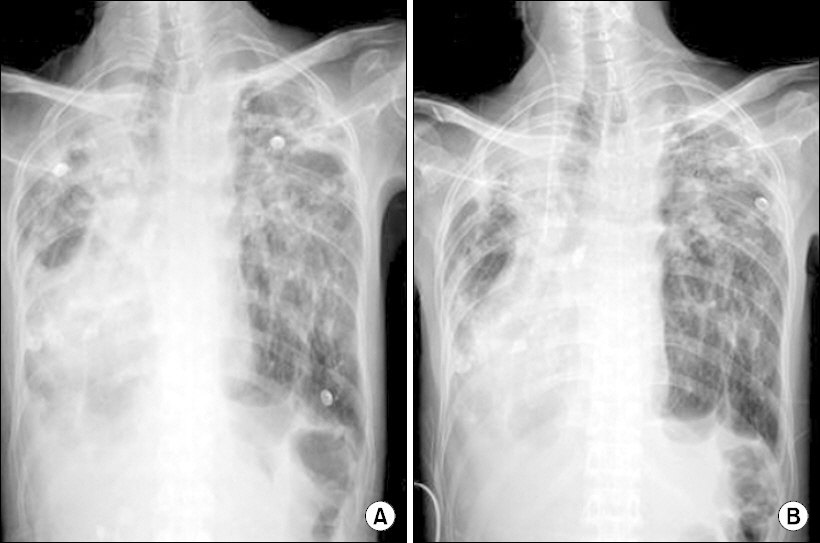
There were no marked differences between preoperative and postoperative chest radiographs (Fig. 2). On postoperative day (POD) 0 in the ICU, pain (NRS, 0Ōł╝3) and RR (18Ōł╝24 beats/min) were well controlled under epidural PCA as the level of anesthesia decreased. On POD 1, oxygen continued to be given via a nasal cannula at 3 L/min, and the patientŌĆÖs NRS was 0Ōł╝2 and RR was 18Ōł╝25 beats/min. ABGA showed pH 7.29, PaCO2 69.8 mmHg, PaO2 53.9 mmHg, and HCO3- 28.1 mmol/L. Cardiac echography performed on POD 1 did not show changes to the RV hypokinesia and severe PH compared to the preoperative conditions. On POD 2, the patient showed mental drowsiness, and ABGA revealed pH 7.27, PaCO2 75.1 mmHg, PaO2 31.6 mmHg, and HCO3- 27.6 mmol/L, with a reduction in RR to 12Ōł╝15 beats/min.
Epidural PCA was immediately turned off, and Biphasic Intermittent Positive Airway Pressure (BIPAP) ventilation was administered and endotracheal intubation prepared (positive end-expiratory pressure 5 cmH2O, pressure support 7 cmH2O, fraction of inspired oxygen 0.3). Target PaO2 and PaCO2 were 40 mmHg and 60 mmHg, respectively. ABGA on POD 3 showed pH 7.3, PaCO2 73.8 mmHg, PaO2 68.8 mmHg, and HCO3- 30.9 mmol/L, while that on POD 4 showed pH 7.38, PaCO2 68.8 mmHg, PaO2 52.5 mmHg, and HCO3- 36.9 mmol/L, suggesting an improvement. On POD 4, the patient complained of pain (NRS 6 once), and morphine 3 mg was intravenously administered. As the patientŌĆÖs RR decreased and the patient showed mental drowsiness again, her pain levels were controlled using nonsteroidal anti-inflammatory drugs. The patient improved from POD 5, POD 6, and POD 7 respectively, with improvements noted in pH (7.38-7.43-7.47), PaCO2 (68.8-59.2-56.9 mmHg), and PaO2 (68.8-59.2-56.9 mmHg), and was transferred to a nearby hospital.
Discussion
Anesthetic management for patients with severe PH has been extensively studied and reported [3,5]. We performed regional anesthesia on a patient with severe PH, using the recommendations provided by previous studies [2]. Further, we performed epidural analgesia for pain control to prevent the exacerbation of RV failure caused by surgical stress and postoperative pain [3]. However, the patientŌĆÖs CO2 retention continued to deteriorate compared to preoperative conditions, which was safely recovered through BIPAP ventilation. In other words, this case is worthy of reporting, as CO2 retention was exacerbated in a patient with chronic cor pulmonale with severe PH even after an adequate level of regional anesthesia was achieved.
Compared to the preoperative PaCO2 (51.6 mmHg), the patientŌĆÖs CO2 levels continued to rise, with PaCO2 reaching 59.4 mmHg intraoperatively and 66.4 mmHg immediately following surgery. Although we continuously confirmed that the spinal block did not rise above the T8 level intraoperatively, there is a possibility that the anesthetic level impaired the ventilatory function by inducing respiratory muscle weakness. It is well known that respiratory function during spinal anesthesia may induce respiratory depression by affecting rib cage movement and abdominal wall movement [6]. This would not pose a serious problem for healthy patients, but spinal anesthesia has the potential to critically effect the ventilatory function in patients with chronic cor pulmonale such as the patient in this case.
Another factor to consider is the possibility of excessive oxygen therapy during surgery. The patient was receiving chronic home oxygen therapy at 1.5 LŌł╝3 L/min via a nasal cannula. The patientŌĆÖs PaO2 on the morning of the operation was 72.2 mmHg. It has been reported that excessive oxygen therapy for patients with chronic pulmonary disease exacerbates CO2 retention by decreasing ventilatory responses [7]. An intraoperative switch to a facial mask with a 4 L/min reservoir from 3 L/min of oxygen via a nasal cannula for safety during anesthesia might have actually induced CO2 retention during surgery. In fact, the patientŌĆÖs intraoperative PaO2 was 217 mmHg, which is about a three-fold increase from her preoperative PaO2, and considering the patientŌĆÖs history of cor pulmonale, this might have been the cause of CO2 retention.
Finally, the most important issue related to the patientŌĆÖs CO2 retention is epidural opioid analgesia. This is because the patient was an opioid na├»ve patient; continuous infusion of epidural PCA was commenced intraoperatively, and PaCO2 gradually increased until POD 2 where PaCO2 reached 75.1 mmHg, while the RR decreased. Further, considering the event in which the patientŌĆÖs CO2 retention suddenly peaked with IV infusion of 3 mg morphine while she was gradually improving and her CO2 levels reduced after the epidural PCA was turned off and BIPAP ventilation was applied, we could speculate that the epidural fentanyl might have been the most likely cause of CO2 retention in our patient with chronic cor pulmonale. Epidural fentanyl has been known to decrease ventilatory response [8], and the optimal dose remains controversial. The guideline protocol from a previous study recommends the use of epidural fentanyl at a base rate of 0.008Ōł╝0.17 ╬╝g┬Ękg-1┬Ęmin-1 [9]. However, in our case, epidural fentanyl was continuously infused at 2.5 ╬╝g/h, which was only a small fraction of the recommended dose. Despite the low dose, epidural fentanyl may still have caused the CO2 retention due to the patientŌĆÖs chronic pulmonary disease with cor pulmonale as well as her sensitivity to opioids.
Finally, the appropriateness of the management at ICU, i.e., performing BIPAP ventilation and not using naloxone, should be reviewed. Based on the reports of a previous study where early use of non-invasive ventilation was effective in chronic obstructive pulmonary disease [10], our decision to apply BIPAP ventilation early in this patient presenting with cor pulmonale which is a chronic pulmonary disease, was appropriate. At the same time, we chose not to use naloxone because the patientŌĆÖs condition was not life-threatening, and activation of the sympathetic nervous system might have exacerbated the patientŌĆÖs right heart failure. As a result, although CO2 retention progressed, we were able to facilitate recovery to the preoperative status by applying BIPAP ventilation before the symptoms progressed to a critical condition.
In conclusion, as previous studies have recommended, regional anesthesia is recommended for non-cardiac surgery in patients with chronic cor pulmonale accompanied by severe PH. However, as demonstrated in our case, even a mild increase in the anesthetic level may cause complications, and an excessive oxygen level may also be inappropriate. In addition, a low epidural opioid dose may decrease the patientŌĆÖs ventilatory response. This case is meaningful as it is the first report that provides insight into the factors that must be considered during non-cardiac surgery of patients with chronic cor pulmonale accompanied by severe PH. In these patients, we recommend anesthesiologists perform regional anesthesia with an appropriate anesthetic level, avoid excessive oxygen, and adequately use epidural analgesia using local anesthetics alone without opioids.